Get Dexur’s Personalized Hospital Specific Presentation on Quality, Safety, Compliance & Education
These articles are part of the Dexur Quality Sights Newsletter, which is focused on Hospital Quality and Safety topics and is read by CEOs, CMOs, CNOs, CQOs, Quality, Safety, Compliance, Analytics & Performance teams. Please email dexurqualitysights@dexur5.com to join this newsletter and receive updates (not more than once per week).
Dexur Hospital Insights
Imagine you're in a routine leadership meeting, presenting your hospital's latest quality metrics from your internal dashboard—readmission rates, and mortality metrics, all seemingly well under control. The team is satisfied and confident in the data's accuracy and the hospital’s performance. Fast forward to the release of the Centers for Medicare & Medicaid Services (CMS) final results, and the situation unfolds quite differently. Suddenly, there’s a stark contrast—CMS data indicates a decline in performance. The board is stunned, the C-suite is questioning the data, and you're left wondering where the discrepancy lies.
Read moreMedical coding and quality improvement teams can effectively leverage data on risk factors that influence specific readmission and mortality measures to enhance healthcare outcomes. By ensuring accurate medical coding, these teams can identify discrepancies and opportunities for improvement, leading to more precise documentation and better resource allocation. Quality improvement teams can utilize this data to target interventions for high-risk patient cohorts, thereby reducing readmission rates and improving care quality. Collaboration between coding and quality teams, informed by comprehensive risk factor analysis, is crucial in driving operational efficiencies and enhancing patient care. This synergy not only supports financial performance through improved coding and reimbursement accuracy but also fosters a culture of continuous quality improvement within healthcare organizations.
Read more48% of SSI Colon Hospital Acquired infections are likely to occur within 10 days of Admission
Importance and Background on Surgical Site Infections in the Colon
Surgical Site Infections (SSI) following colon surgery present a significant challenge in healthcare. They adversely affect patient recovery and impact hospital quality metrics. These infections not only lead to longer hospital stays and increased costs but can also result in severe, life-threatening complications. Therefore, it is essential to focus on enhancing infection control measures and implementing robust post-surgical care protocols to effectively prevent and manage these infections.
Read moreThis white paper highlights how healthcare organizations can significantly reduce costs and enhance operational efficiency by consolidating multiple functions into a single platform with Dexur's AI Unified Quality and Risk Management software. Dexur offers an AI-powered unified system for managing quality, safety, risk, and incidents. By adopting Dexur's integrated software, healthcare providers can streamline their operations and achieve a higher standard of care at a reduced expense.
Read moreKey Pathogens Influencing CAUTI Infections in Hospitals
Catheter-associated Urinary Tract Infections (CAUTI) greatly influence both patient outcomes and the financial aspects of healthcare, with Dexur being a key contributor in data analytics to improve healthcare safety and quality. Leveraging hospital data reported to the CDC's NHSN, Dexur identifies key pathogens contributing to CAUTI, highlighting the top five: Escherichia coli, Pseudomonas aeruginosa, Klebsiella pneumoniae, Enterococcus faecalis, and Proteus mirabilis. Each of these pathogens poses distinct challenges in their treatment and prevention. Through Dexur's detailed analysis, the development of targeted infection control protocols is facilitated, and the process supports both Root Cause Analysis (RCA) and the implementation of Corrective and Preventive Actions (CAPA). Such a strategy is crucial for the effective management of CAUTI, with the ultimate goal of enhancing patient outcomes and the efficiency of healthcare services.
Read moreThe Texas Hospital Association (THA) has endorsed Dexur, an AI-driven unified Quality, Safety, Risk, and Incident Management software, to support its member hospitals. This partnership is highlighted by THA's Alex Huff and Dexur's CEO, Nik Rao, who emphasize the alignment of Dexur's advanced technological capabilities, including AI-driven analytics and comprehensive data management, with THA's goals for enhancing healthcare quality and efficiency. Dexur's platform will offer THA hospitals a suite of tools for detailed program-to-case analysis, predictive insights, and strategic planning aimed at improving patient care outcomes and operational performance at a dramatically cost-effective price.
Read moreA Significant Portion of Readmitted Patients Stay for only 1 or 2 Days
Readmissions are a critical quality metric for hospitals, significantly impacting financial and reputational outcomes under the Hospital Readmissions Reduction Program (HRRP) and the Centers for Medicare & Medicaid Services (CMS) Star Rating system. The HRRP imposes penalties on hospitals with higher-than-expected readmission rates for specific conditions, aiming to incentivize improvements in hospital discharge planning and post-discharge care. Similarly, the CMS Star Rating system evaluates hospitals on various performance measures, including readmission rates, to help consumers compare hospitals more easily. High readmission rates can lead to reduced Medicare payments and lower star ratings, which may influence patient choice and hospital revenue.
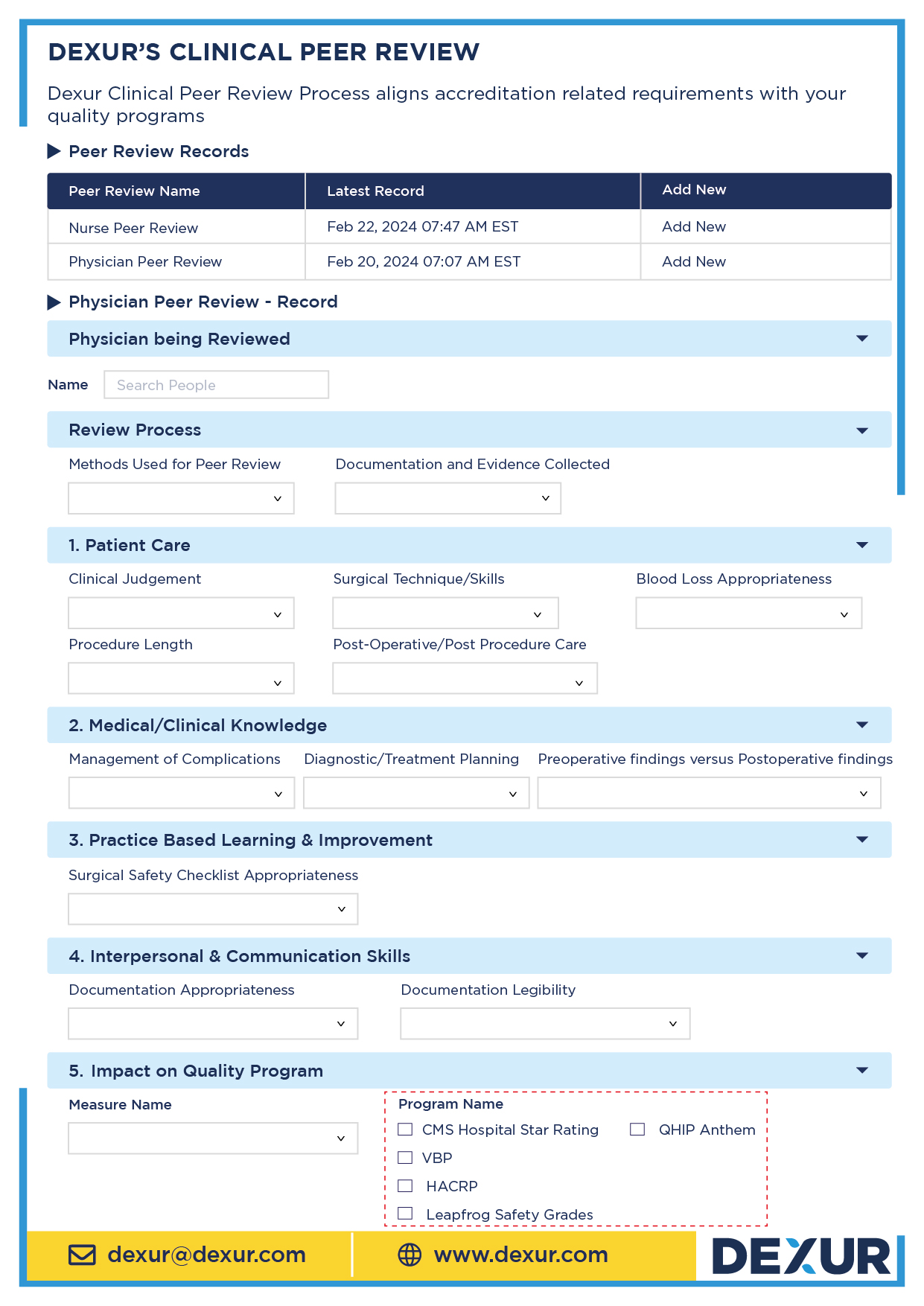
Read morePeer review is a critical component in the accreditation and quality assurance processes for healthcare organizations. The Joint Commission (TJC), the Centers for Medicare & Medicaid Services (CMS), Det Norske Veritas (DNV), and the National Committee for Quality Assurance (NCQA) each have specific expectations regarding peer review processes.
Read moreWebinar: Dexur Releases its Annual 2024 CMS Star Rating Predictions
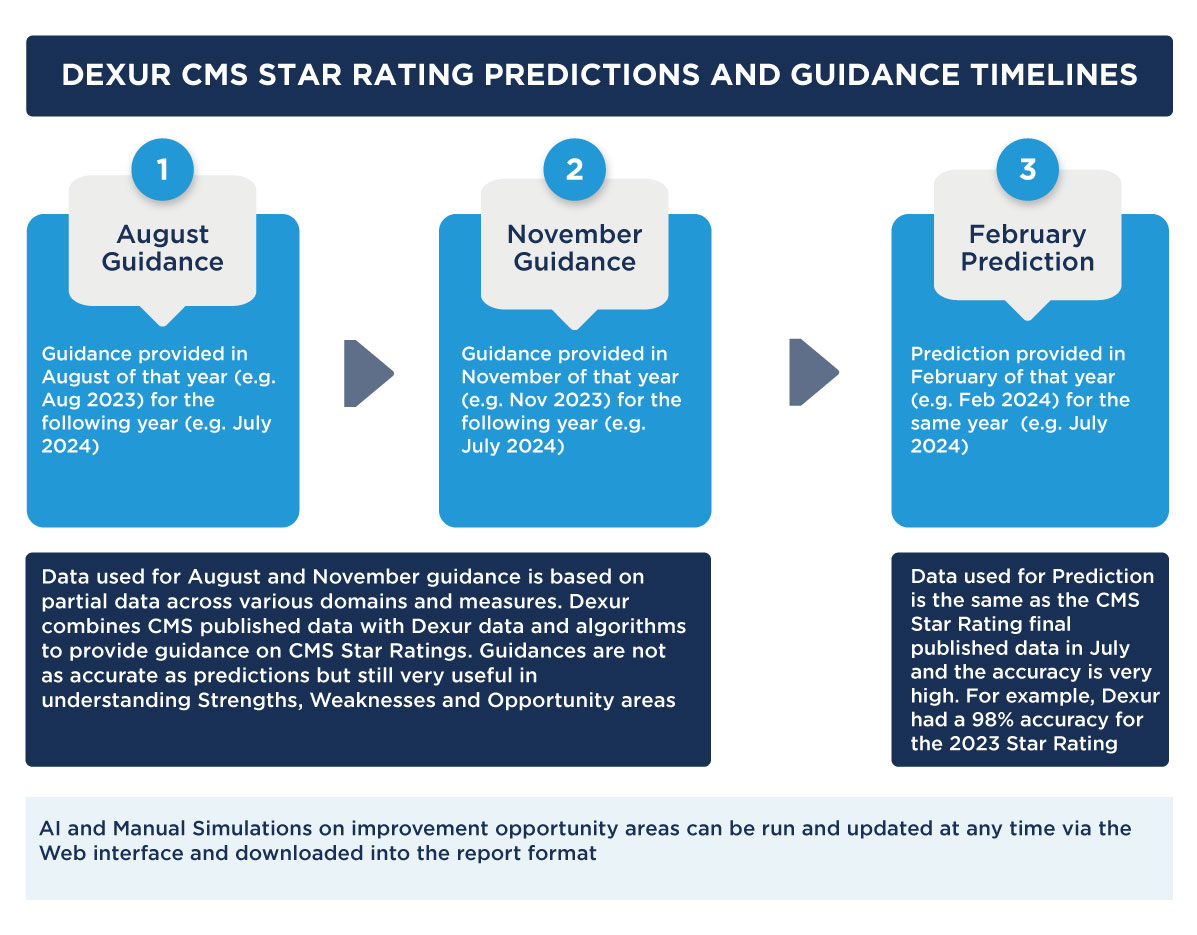
Dexur makes its annual predictions on CMS Star Ratings before CMS Star Ratings are published in July of every year. In 2023, Dexur had a 98% accuracy rate in its annual prediction rate. To get an understanding of your Hospital’s increase in decrease of your Star Rating, you can search for your Hospital’s prediction via the Hospital Search Function or you can also go through any Hospital’s CMS Star Rating predictions direction by browsing through state pages. To get the actual Star Rating prediction and a glimpse of the key drivers of the performance, you can also reach out to Dexur by email dexur@dexur.com.
Read moreEmergency Departments Play a Critical Role In Managing Readmissions
Readmissions to hospitals, particularly within 30 days of discharge, serve as a critical measure for evaluating the quality and effectiveness of healthcare services. The Hospital Readmission Reduction Program (HRRP) and the Centers for Medicare & Medicaid Services (CMS) Star Rating system place significant emphasis on readmission rates as indicators of hospital performance. These measures directly impact hospitals' financial health through penalties and influence their reputation through public reporting.
Read moreWhy are Inpatient THA / TKA Readmissions and Complications Increasing?
Total Hip Arthroplasty (THA) and Total Knee Arthroplasty (TKA) are critical measures in assessing the quality of care provided by healthcare facilities, particularly in the context of Medicare's value-based care models. These procedures are common among the elderly population, who are the primary beneficiaries of Medicare. The rates of 30-day readmission and complications after THA/TKA are significant indicators of the quality and effectiveness of perioperative care, postoperative management, and the overall health system's ability to provide coordinated care. These metrics directly impact various Centers for Medicare & Medicaid Services (CMS) Quality Programs, such as CMS Star Rating and the Hospital Readmissions Reduction Program (HRRP), which penalizes hospitals with higher than expected readmission rates for certain conditions and procedures, including THA/TKA.
Read moreHow the SEP1 Chart Abstraction Measure can be Integrated into CMS Star Ratings and VBP
The SEP1 chart abstraction measure, a critical component in healthcare quality assessment, plays a pivotal role in evaluating the efficiency and effectiveness of sepsis management in healthcare facilities. Sepsis, a life-threatening response to infection leading to tissue damage, organ failure, and potentially death, requires timely and precise treatment. The SEP1 measure is designed to quantify the quality of this treatment by tracking various parameters, such as the timeliness of antibiotic administration and the completeness of sepsis care.
Read moreWhat are the Top Pathogens Impacting CLABSI Infections in Hospitals
Central Line-Associated Bloodstream Infections (CLABSI) remain a significant challenge in healthcare settings, directly influencing patient outcomes and healthcare costs. CLABSI, a severe infection occurring in patients with central venous catheters, poses risks that extend beyond immediate health concerns, impacting hospital ratings and reimbursement rates.
Read moreDexur, a leading provider of AI-driven unified quality and safety, risk, and incident management software, will acquire the Comparative Outcome Profile (COP) chart abstraction software from the Indiana Hospital Association (IHA). This strategic move aims to bolster Dexur's capabilities in offering comprehensive, AI-powered solutions to healthcare organizations.
Read moreMedical coding plays a crucial role in determining risk-adjusted rates, directly influencing a hospital's performance in quality programs like CMS Star Ratings, HRRP, and VBP. Risk adjustment is essential for equitable evaluations, especially in treating complex patient cases. Detailed coding impacts these risk-adjusted metrics, as seen in a case study of Acme Hospital, where coding accuracy significantly affects quality measures and assessments. A comparative analysis of Acme and Vibrant Hospitals further highlights the importance of precise coding practices in reflecting patient care complexity and ensuring fair evaluations in healthcare quality programs.
Read moreHow Saving One AMI Mortality Per Year Can Help a Typical Hospital Move To the Top Percentile
Hospitals across the United States, from rural facilities in rural areas to large-scale Acute Care centers in urban areas, are continually striving to enhance the quality of their services. A key focus for these hospitals is to reduce mortality from AMI (Acute Myocardial Infarction), an essential goal for improving their CMS Star ratings and benefiting from the Value-based Purchasing (VBP) program. This objective is a significant indicator of care quality and heavily influences the mortality group within the CMS Star rating system.
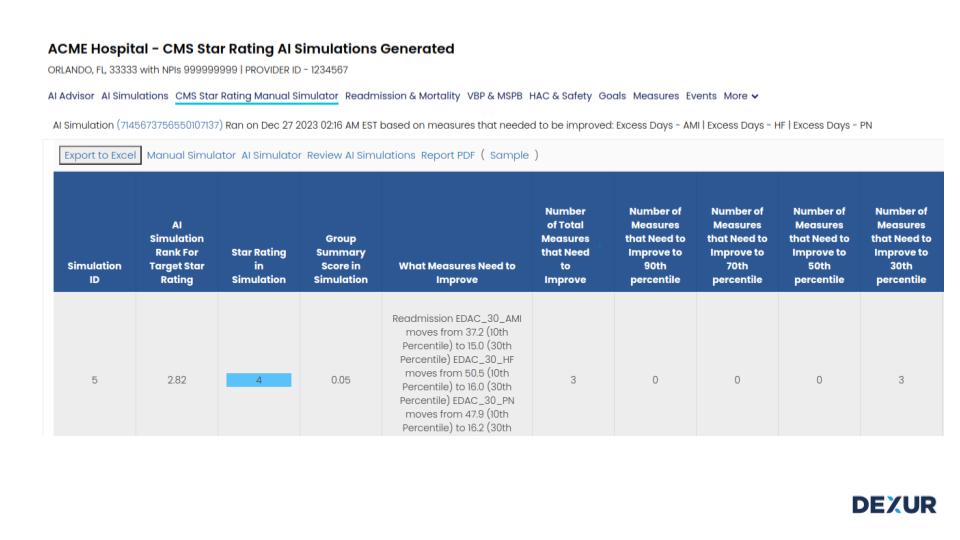
Read moreA Deep Dive into CMS's Excess Days in Acute Care (EDAC) Methodology
The Centers for Medicare & Medicaid Services (CMS) developed the Excess Days in Acute Care (EDAC) methodology as a critical tool for assessing and managing healthcare efficiency, particularly in relation to post-discharge care. This methodology is a significant element in the CMS Star Rating system, especially in the Readmission Group, which carries a substantial weight of 22%. By evaluating excess days spent in acute care settings, EDAC offers insights into the effectiveness of hospital discharge planning and post-discharge care coordination.
Read moreUltrashort Readmissions are 30-40% of CMS 30 Day Readmission Measures
Ultrashort hospital readmissions, defined as patient readmissions within 7 days of discharge, present a significant challenge in healthcare management. These early readmissions not only reflect on the quality of care provided but also have substantial implications for patient safety and healthcare costs.
Read moreCLABSI Case Study: Integrating Safety Huddles & Best Practices with Risk & Incident Management
Central Line-Associated Bloodstream Infections (CLABSIs) present a significant challenge in healthcare settings, critically impacting patient safety and care quality. These infections, often associated with the use of central lines in medical treatments, pose substantial risks, influencing key quality measures such as the NHSN (National Healthcare Safety Network) CLABSI metrics. This metric is integral to quality programs like the CMS Hospital CMS Star Rating, Hospital-Acquired Condition Reduction Program (HACRP). Leapfrog and other quality programs that influence hospital ratings and funding. CLABSIs are not only a patient safety risk concern but also a quality indicator, affecting a hospital's performance evaluation and reputation.
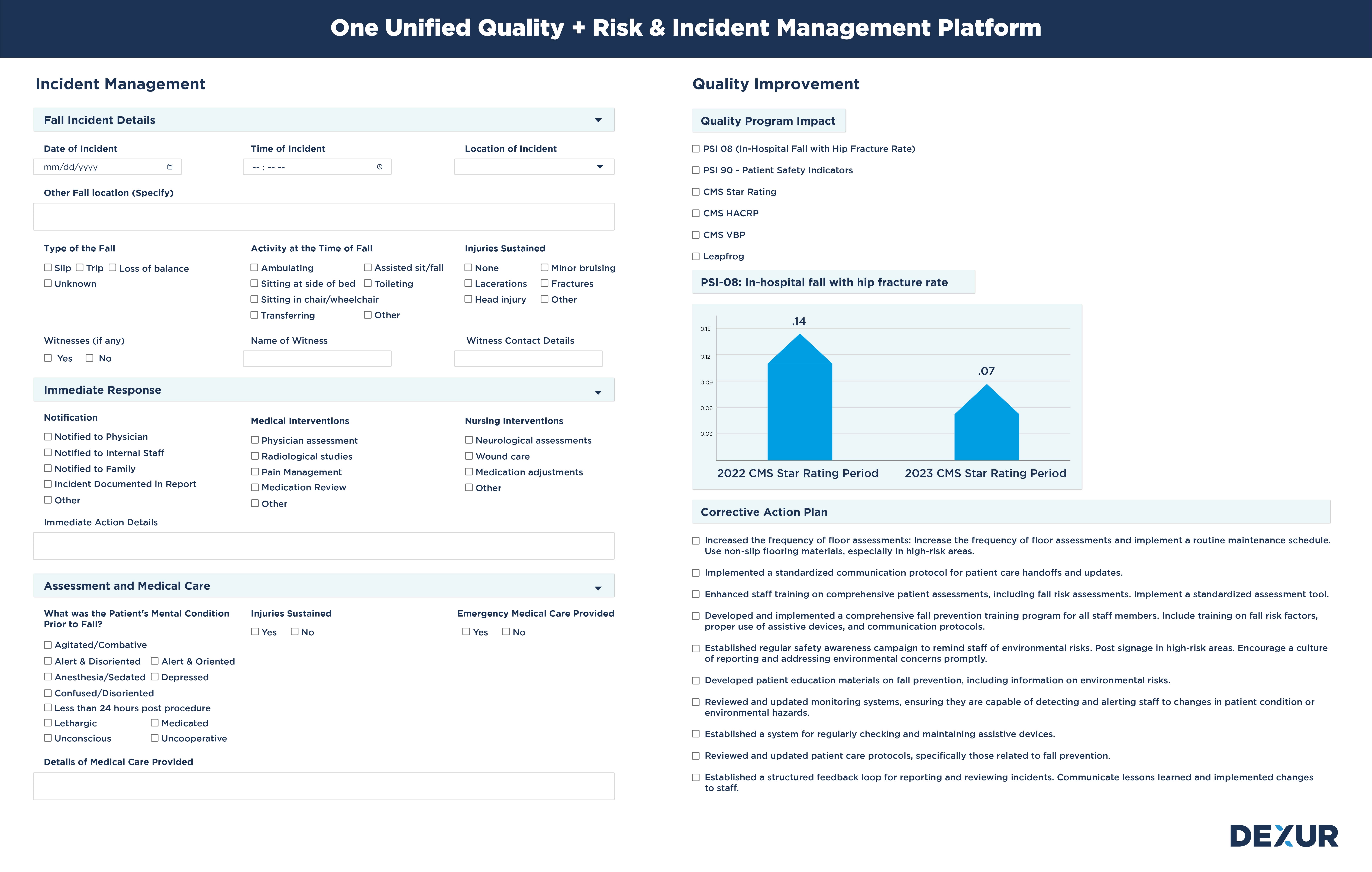
Read morePatient Falls: Case Study: Quality and Risk are Two Sides of the Same Coin
Patient falls within healthcare settings are a significant concern due to their implications on patient safety and quality of care. These incidents have an impact on risk management and also have an impact on measures like PSI 08 (In-Hospital Fall with Hip Fracture Rate) which is part of PSI 90, which influence crucial quality programs including CMS Star Ratings, the Hospital-Acquired Condition Reduction Program (HACRP), and Leapfrog standards. PSI 90, or the Patient Safety and Adverse Events Composite, encompasses a range of hospital-acquired conditions, among which patient falls are a critical component. The impact of falls on these quality measures is profound, as they directly affect a hospital's reputation, funding, and overall performance evaluation.
Read moreThe Big Picture in Infection Prevention: Beyond Day-to-Day Operations
Infection Prevention teams in hospitals play a critical role in maintaining patient safety and healthcare quality. Their work, often seen through the lens of daily tasks and immediate outcomes, holds a far greater significance in the broader context of healthcare delivery and institutional reputation. To fully grasp the impact of their efforts, it's essential for these teams to understand the big picture, much like the famous story of a civil engineer who, when asked about their job, said they were not just building walls and roofs but a beautiful building. This narrative underscores the importance of seeing beyond the immediate task to appreciate the larger purpose and impact of one’s work.
Read moreHospitals Need To Introduce and Adopt The Concept of Readmission and Mortality Huddles
Hospitals seeking to enhance healthcare quality and patient safety have adopted strategies like the 'Safety Huddle,' a collaborative session focusing on patient safety concerns. Evolving from this concept is the 'Readmission and Mortality Huddle,' an interdisciplinary team meeting specifically aimed at analyzing readmissions and mortalities. This focused approach is crucial in the light of Dexur's findings about the narrow scope for improvements in healthcare metrics. The goal of these huddles is to identify patterns, discern root causes, and devise prevention strategies, with frequent and concise meetings enabling prompt interventions and ongoing monitoring, marking a significant advancement in hospital management.
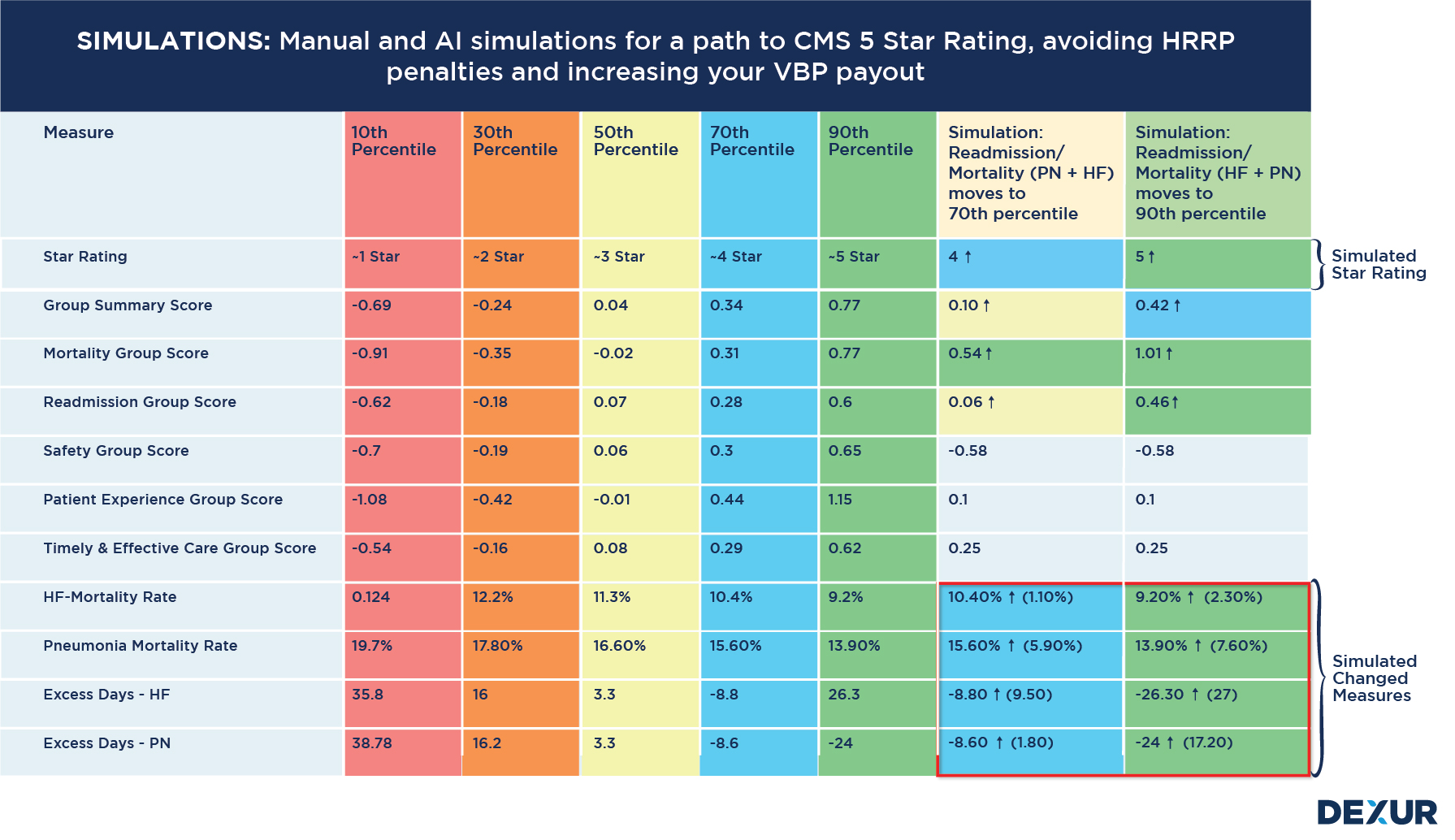
Read moreDexur's AI Advisor Shows Quality Improvement is a Game of Inches
Dexur had already previously published that the difference between the Bottom 10th & top 90th Performance Percentiles of CMS Readmission and Mortality Measures is Very Small. Dexur’s AI Advisor can automatically analyze a Hospital’s data and give very specific goals and counts on what it takes for Hospitals to get to the top 90th percentile. Dexur’s AI Advisor's findings suggest that for many hospitals, reducing readmissions and mortalities by less than 10 per year can significantly boost their percentile ranking. This revelation is crucial as it indicates that even minor improvements can lead to substantial gains in a hospital's performance metrics.
Read moreHospital Incident Management Systems: A Wasted Opportunity to Integrate Quality Metrics
Hospital Incident Management Systems are widely adopted across healthcare organizations to capture, track, and manage events that could potentially harm patients, employees, or the institution. Although these systems play a crucial role in identifying and mitigating risk, they often function in isolation from Quality Management Systems. As a result, there's a missed opportunity to integrate quality goals and measures such as the CMS Star Rating, Leapfrog Hospital Safety Grade, Hospital Readmissions Reduction Program (HRRP), Hospital-Acquired Condition Reduction Program (HACRP), and Value-Based Purchasing (VBP).
Read moreSynchronizing Anthem QHIP and CMS Quality Programs for Unified Improvement
Anthem Quality-In-Sights Hospital Incentive Program (QHIP) and CMS's Star Rating and Hospital Readmission Reduction Program (HRRP) have designed several measurement programs with commendable intentions, the measures frequently result in hospitals addressing them in isolation, potentially due to varied reporting requirements and benchmarks. Herein lies the opportunity for creating a system that unites these common measures to optimize efforts, resources, and ultimately, patient care. Some common measures and thier groupings among Anthem QHIP, CMS Star Ratings and HRRP include:
Read moreHow Much Time is Left for Impacting 2025 & 2026 CMS Star Rating Measures?
Hospital quality teams aspire to formulate plans that exert Impact over CMS Star Ratings, necessitating both short-term and long-term strategies. A sustainable, long-term game plan would likely encompass comprehensive, AI-driven simulations to comprehend the most effective path toward an enhanced star rating. Nevertheless, hospitals might also encounter pressure to yield results in the short term.
Read more9 Ways Hospital Quality Teams Go Astray With Internal Dashboards and Tracking
Introduction: Hospitals rely on internal quality dashboards to track various measures aimed at improvement in CMS Star Ratings, VBP, Leapfrog, HRRP, HACRP, and other programs. However, despite these efforts, several inherent challenges in the current systems can lead hospitals astray. Dexur offers an innovative solution by combining internal data with its proprietary data and utilizing best-in-class scoreboard tracking algorithms, thereby presenting a more comprehensive and true picture of hospital quality.
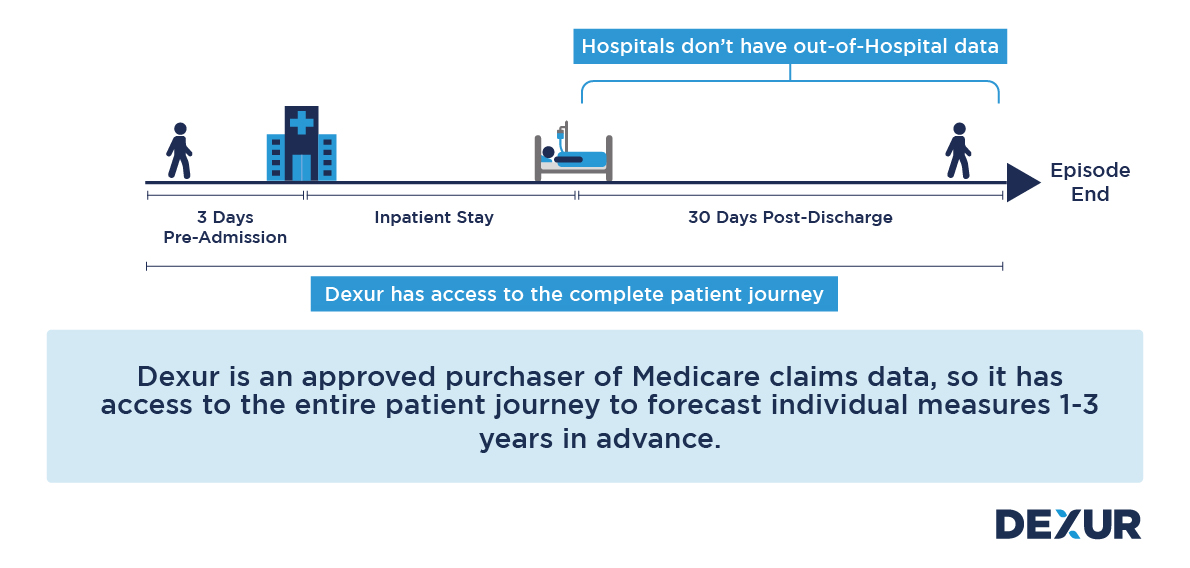
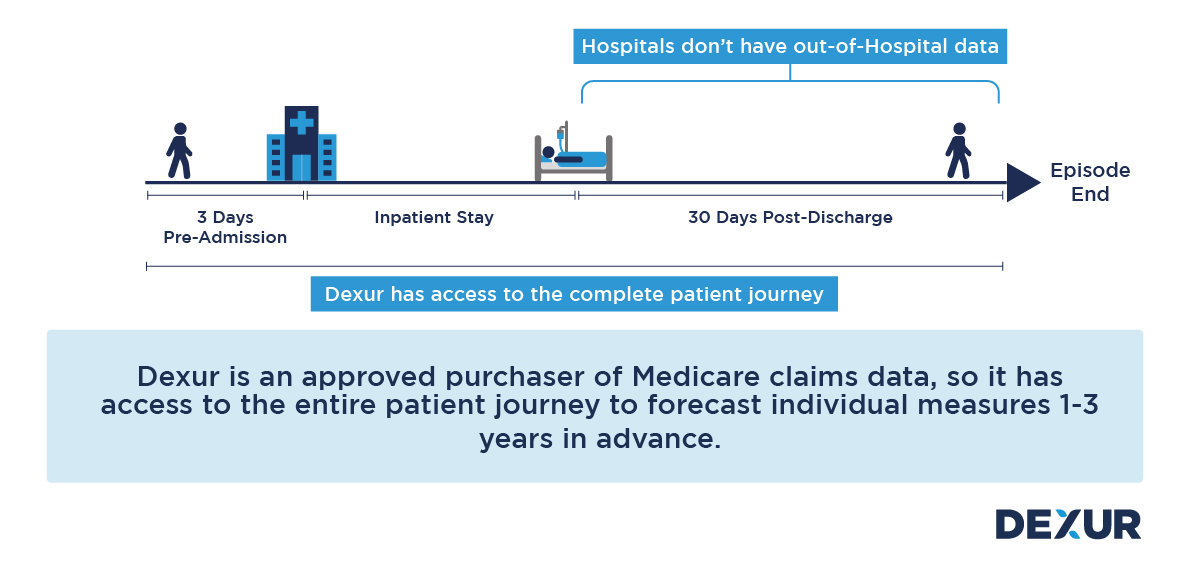
Read moreThe Medicare Spending per Beneficiary MSPB measure is designed to assess the average spending per Medicare beneficiary, which is indicative of the efficiency and cost-effectiveness of a hospital or healthcare provider. By evaluating the total cost of services rendered during an MSPB episode, which includes the inpatient stay, 3 Days before the Inpatient Stay and the 30 days following discharge, CMS aims to identify variations in spending, incentivize cost reduction, and promote high-quality care.
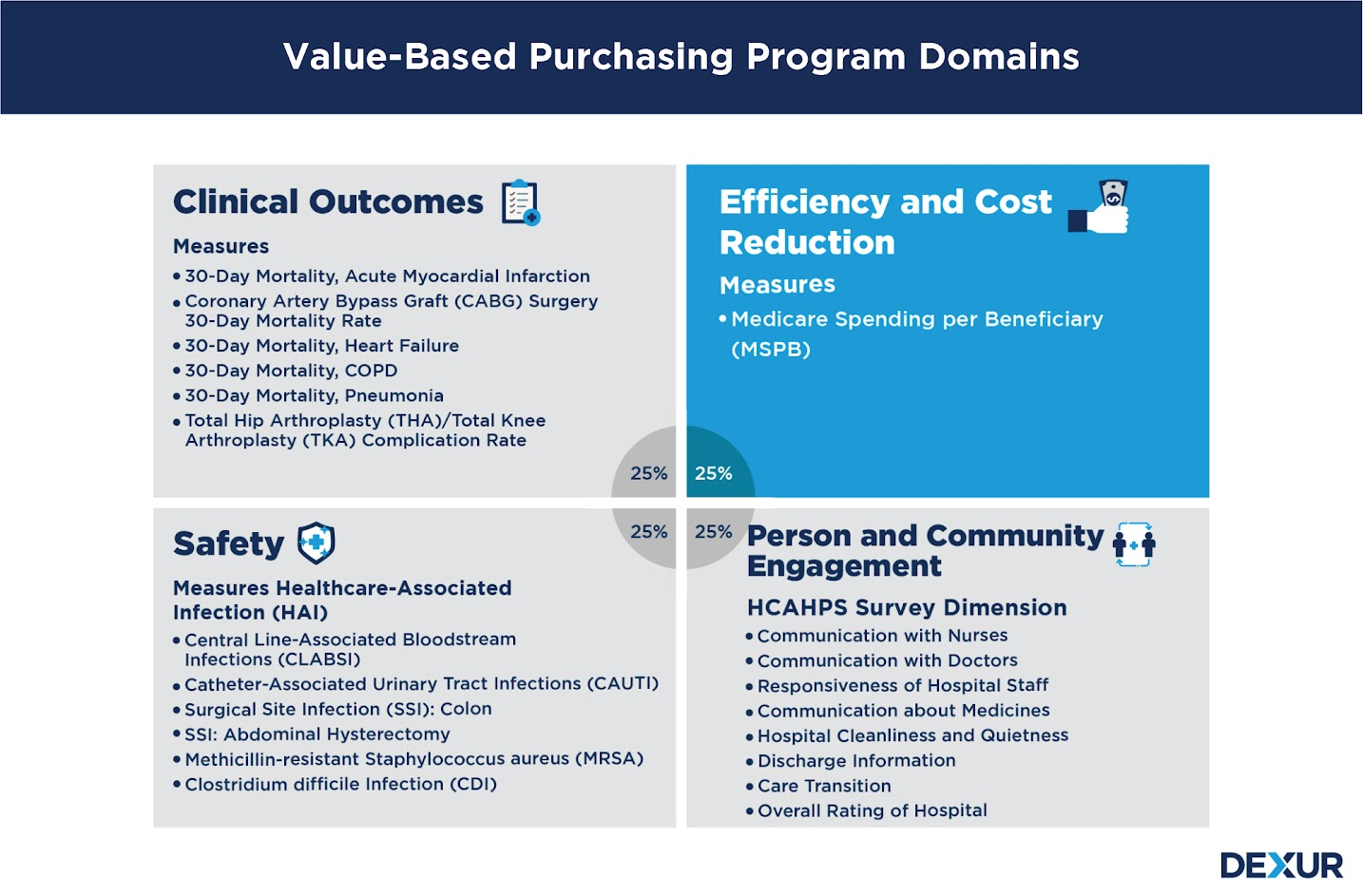
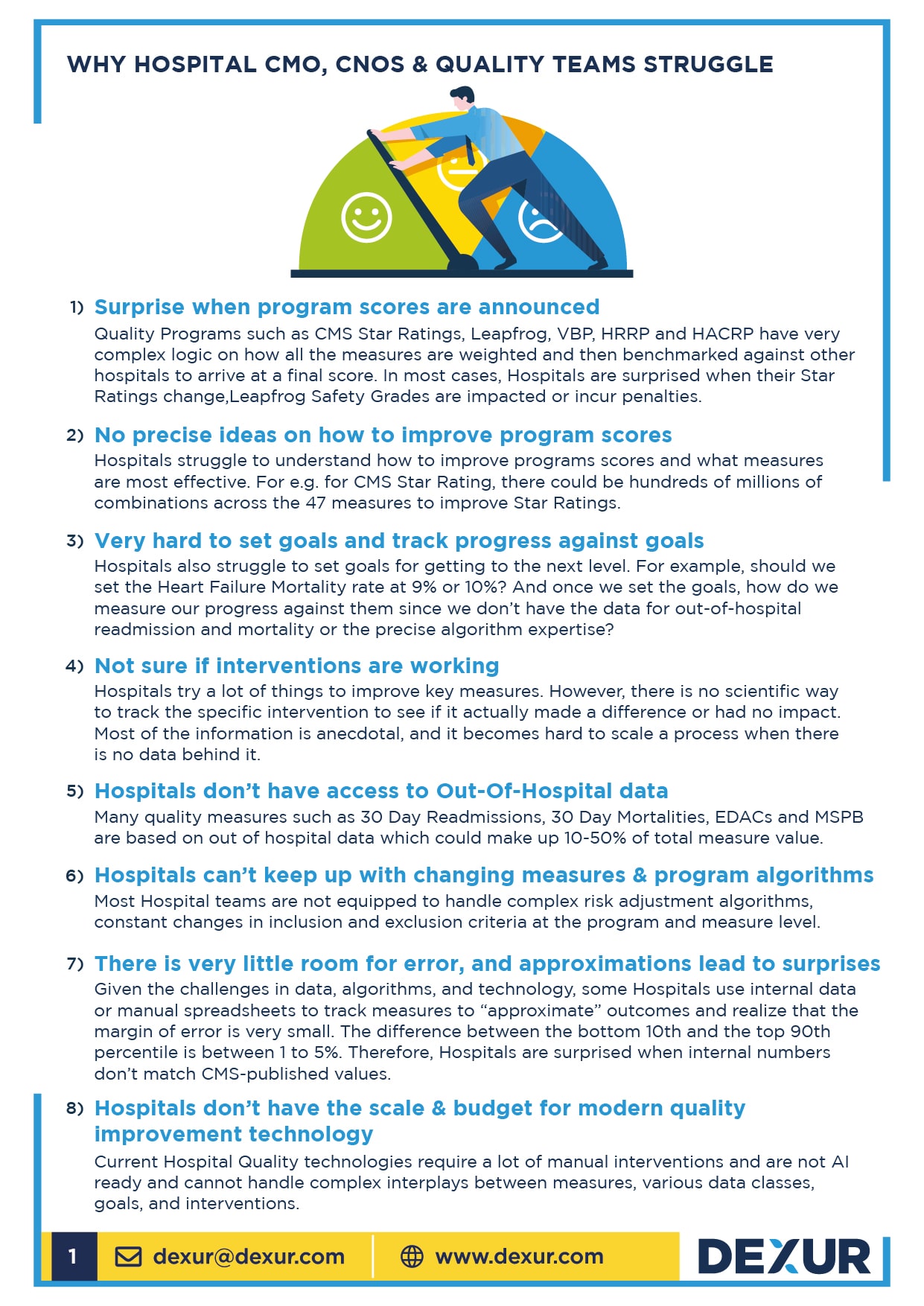
Read moreThe article outlines eight challenges faced by CMOs, CNOs, and Quality Teams in managing hospital Quality Programs. Hospitals often grapple with unpredicted program score changes due to complex scoring mechanisms. Moreover, they struggle to pinpoint improvement strategies from myriad possible measures, find it hard to set and track progress towards goals, and remain uncertain about intervention efficacy. Additionally, the lack of access to out-of-hospital data, the rapidly changing nature of program measures, a slim margin for error in data approximations, and the inability to invest in advanced quality improvement technologies further complicate their endeavors to enhance care quality.
Read moreHow To Integrate Your Leapfrog and CMS Star Rating, VBP and HACRP Quality Improvement Initiatives
Quality and safety measures have long been at the forefront of healthcare, ensuring that hospitals provide optimal care to their patients. Two significant entities, The Leapfrog Group and the Centers for Medicare & Medicaid Services (CMS), have instituted multiple programs to monitor and assess these measures. Though these programs have several overlapping measures, hospitals often tackle them individually, leading to potential inefficiencies. Dexur's innovative approach, using AI simulations and calculators, offers a consolidated strategy for hospitals to improve upon these common measures.
Read moreHarnessing AI for Early Warning Alerts in Hospital Quality Metrics
Every day, hospitals and healthcare systems grapple with hundreds of quality measures that impact critical quality programs like CMS Star Rating, VBP, HRRP, and Leapfrog. These measures, encompassing everything from mortality and readmission rates to HCAHPS Patient experience measures, are pivotal in determining patient care strategies, upholding hospital reputation, and clinching significant financial incentives.
Read moreCMS Mortality measures are a critical part of CMS Star Ratings (~22% of overall weightage) and VBP (~25% of Weightage). Within the CMS Mortality measures, Pneumonia, HF, AMI and COPD are the most common measures in Mortality. A big gap while Hospitals try to measure 30 Day mortality is that Hospitals are blind to what happens outside their walls and nearly 60% of deaths are outside the Index Stay. Since, Dexur is an approved purchaser of Medicare Claims data, we can provide insights into what happens out of the Index stay and how what percentage of patient deaths can be potentially impacted.
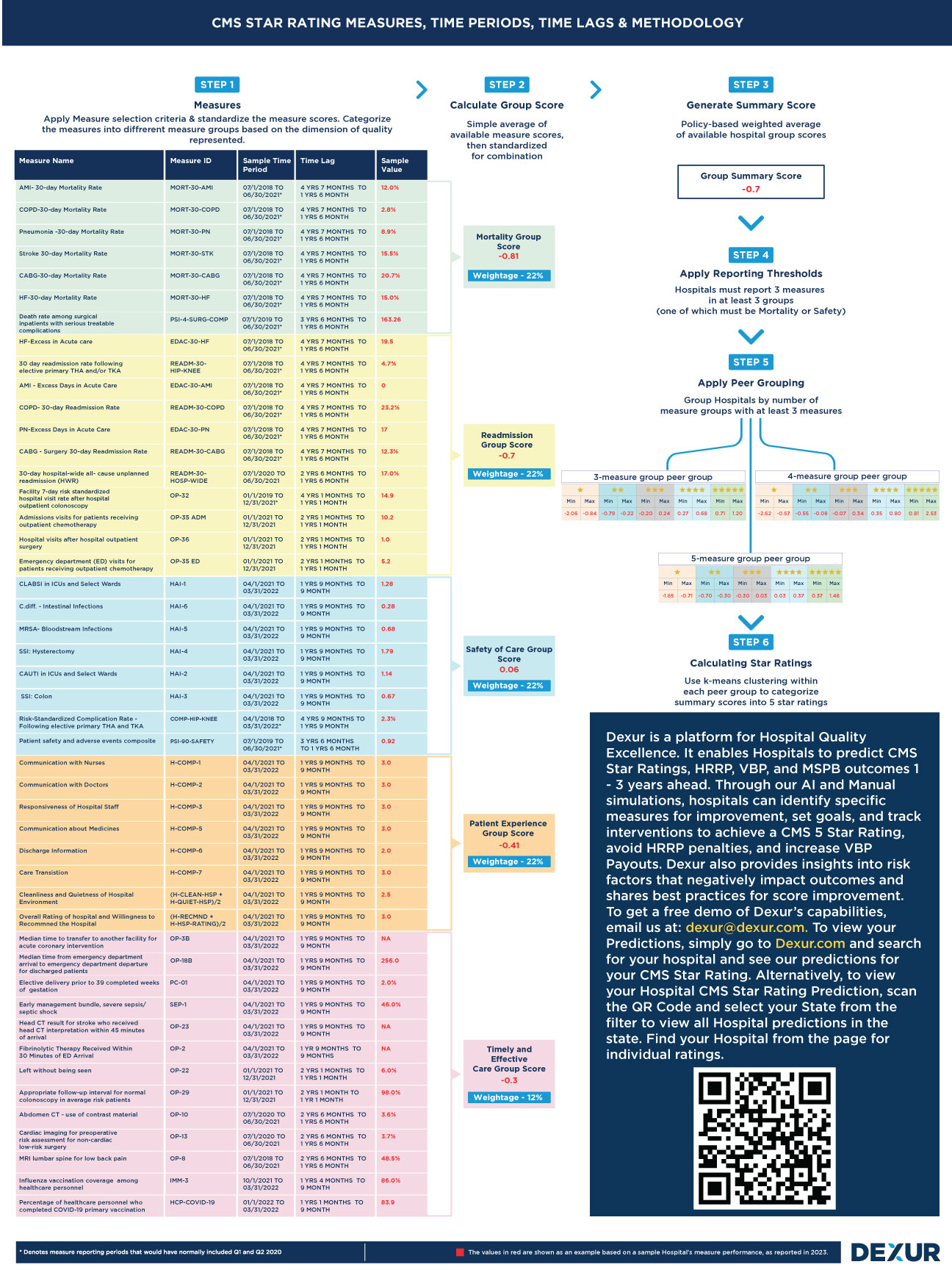
Read moreDexur’s Free CMS Star Rating Measures, Time Periods, Time Lags and Methodology Poster
The Hospital CMS Star Ratings, designed to measure the quality of healthcare institutions, often presents hospitals with the challenging task of comprehending its intricate methodologies, encompassing performance periods, time lags, and specific weightages of different measures. Dexur, recognizing the complexity of these ratings, has identified that a significant portion of their interactions with hospitals revolves around elucidating these aspects. The need for clarity becomes particularly pronounced when considering that various teams within hospitals - from top-tier executives like the CEO, COO, CMO, CQO, and CNO to the Quality Departments - often have divergent understandings of how the Star Ratings function.
Read moreDexur’s 2024 CMS Star Rating Guidance in August 2023 is now available
Dexur’s 2024 Star Rating August 2023 Guidance is now available for hospitals and healthcare providers to review. Dexur has a 98% accuracy rate for its predictions in February. Our guidances, based on partial data, are less accurate but are still very useful to understand directionality, strengths, weaknesses and opportunities. Dexur customers may have a different guidance than what is shared below because they may have provided additional data to use in our guidance model.
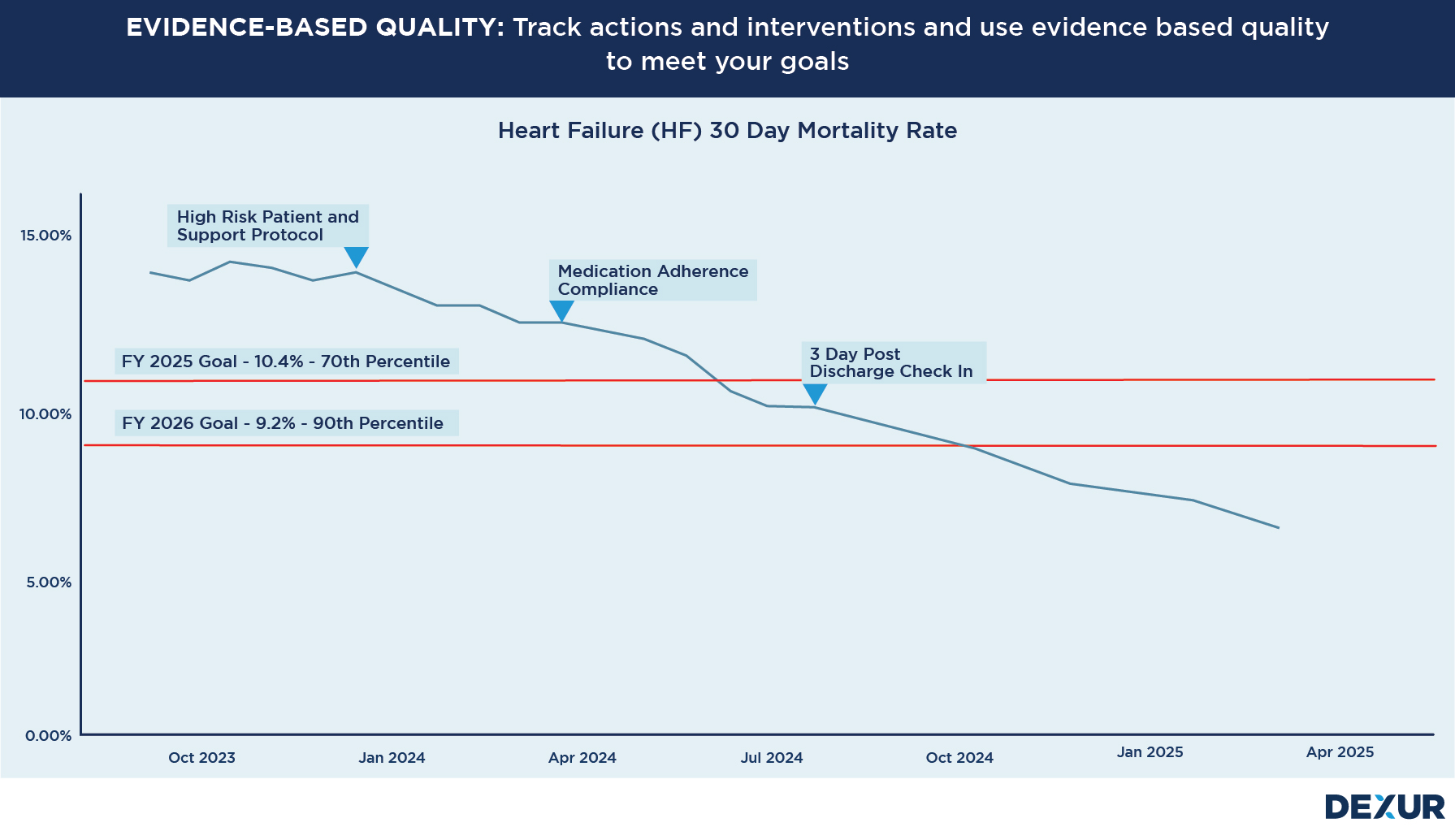
Read moreIn the vast expanse of the healthcare landscape, where patient care and hospital reputation are inextricably linked, hospitals frequently deploy a myriad of quality improvement initiatives, interventions, and actions. The goal is clear: to enhance the quality of care and ensure that patients receive the best possible treatment outcomes. However, there’s an underlining challenge that Chief Medical Officers (CMOs), Chief Nursing Officers (CNOs), and Quality Teams often grapple with — How do we know if these interventions are genuinely working?
Read moreNearly 30% of Readmissions are to a Different Hospital From the Index Stay
Hospitals face challenges in tracking CMS (Centers for Medicare & Medicaid Services) 30-Day readmissions due to the limitations of data. The 30-day Readmission measure is calculated based on the number of patients who are readmitted within 30 days of their initial hospital admission. However, hospitals lack access to comprehensive out-of-hospital information, making it difficult for them to track these measures accurately. Dexur is an approved purchaser of Medicare claims data and which allows it to evaluate patient outcomes, identify patterns and trends, and provide a more complete picture of healthcare utilization and performance. This data can be instrumental in identifying areas for improvement, developing strategies to reduce mortality and readmissions, optimizing resource allocation, and enhancing the overall quality of care.
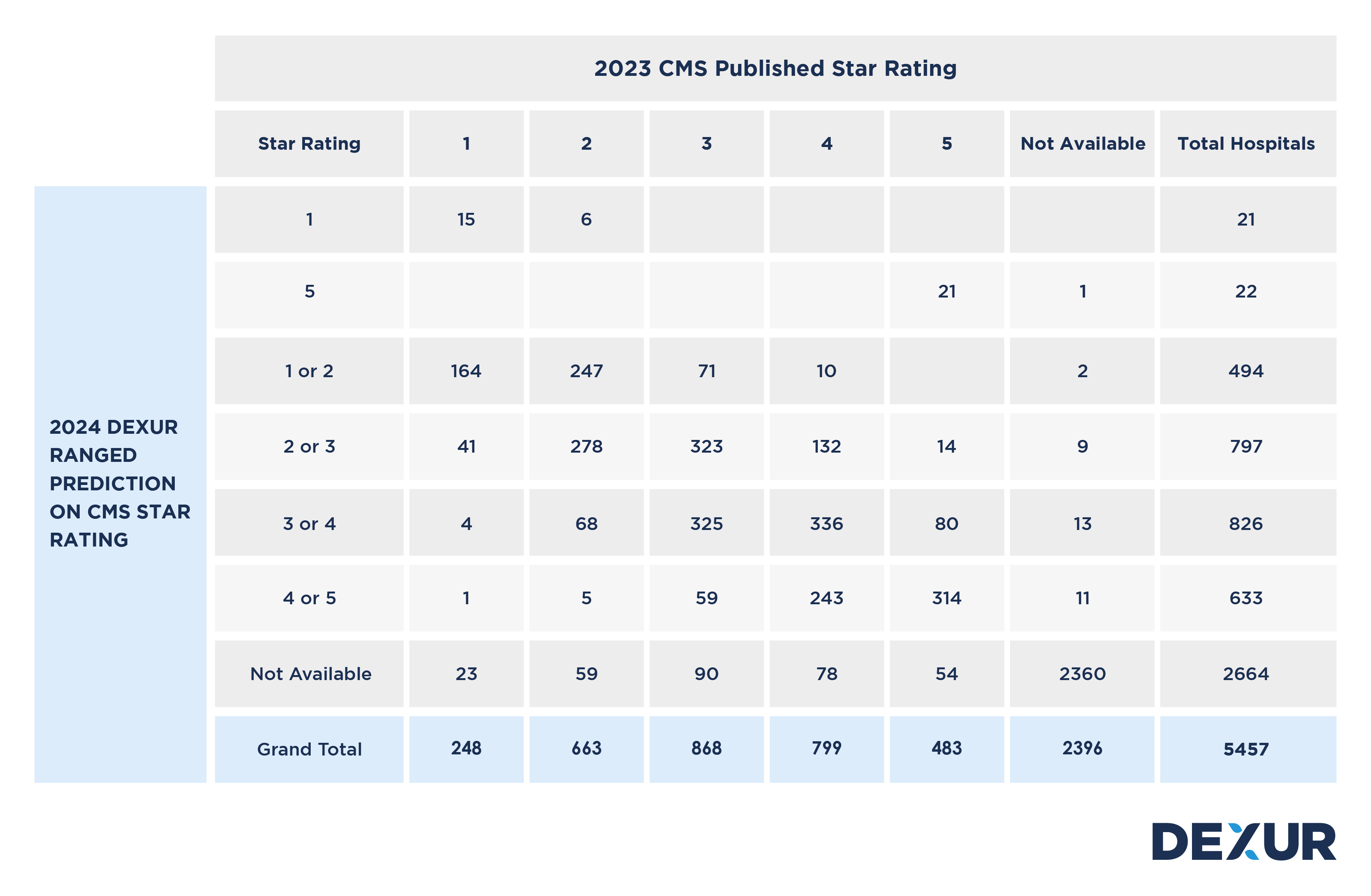
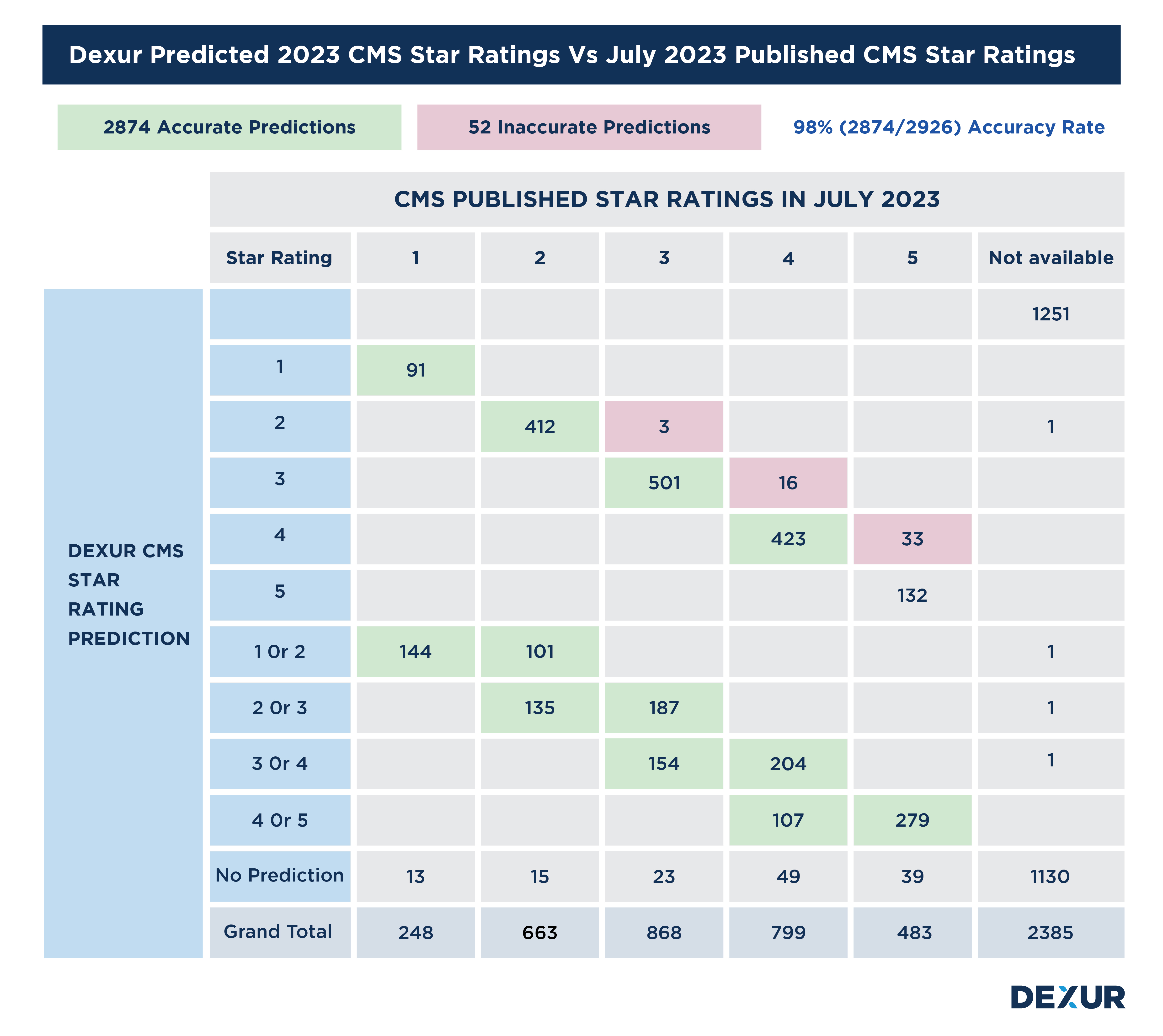
Read moreDexur has a 98% predictive accuracy in 2023 CMS Star Ratings
CMS just released its 2023 CMS Star Ratings on July 26, 2023. Based on the data files, released Dexur compared its CMS Star Rating predictions made in Jan / Feb 2023 to actual CMS published files and the details of comparison are shown below.
The key stats are given below:
-
Dexur made a prediction on 2926 Hospitals
-
Dexur correctly forecasted the CMS Star Rating in 2874 Hospitals (Green Highlighted in below table)
-
Therefore, Dexur has a 98% (2874/2926) predictive accuracy for 2023 CMS Star Ratings
-
52 Hospitals (Highlighted in pink in the below table) were incorrectly forecasted
Nearly 60% of Deaths for CMS Mortality Measures Happen Outside the Index Stay
Hospitals have a challenge in tracking CMS 30-Day Mortality measures because they try to monitor more real-time information using internal hospital data, which does not have out-of-hospital information used for 30-day mortality and readmission measures. However, Dexur is an approved purchaser of Medicare claims data and, therefore, can analyze the full patient journey that impacts measures such as 30-day mortality, 30-day readmissions, MSPB, and EDAC.
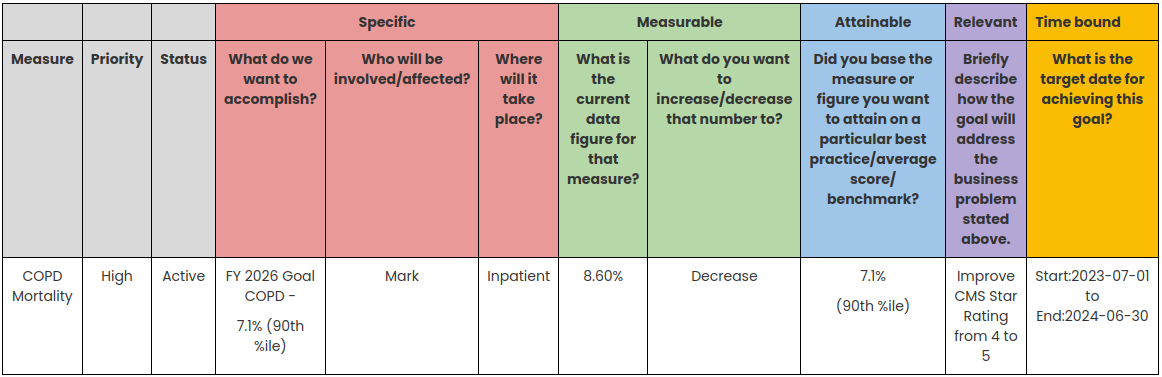
Read moreHow to Integrate CMS QAPI Goal Setting Frameworks for CMS Star Rating, VBP & HRRP
CMS QAPI (Centers for Medicare & Medicaid Services Quality Assurance and Performance Improvement) encourages healthcare organizations to establish and monitor quality improvement goals. These goals can align with the metrics and measures used in CMS quality programs, including Star Ratings, VBP and HRRP. By setting specific goals to improve performance on quality measures that impact Star Ratings VBP and HRRP, healthcare organizations can directly link their compliance efforts to the desired outcomes in CMS quality programs.
Read moreIn the pursuit of improving healthcare quality and patient outcomes, the Centers for Medicare & Medicaid Services (CMS) rely on various measures to evaluate the performance of hospitals and healthcare providers. Two crucial indicators that have garnered significant attention to assess hospital performance are readmission and mortality rates. These measures are crucial in measuring Hospitals’ performance in various CMS quality programs. For instance, readmissions and mortality measures constitute 44% weightage in the calculation of CMS Star Ratings, and readmissions are the sole driver of the Hospital Readmissions Reduction Program (HRRP).
Read more