Medicare Spending per Beneficiary (MSPB) 101: What is it? What is Included? And How is it Calculated?
Get Dexur’s Personalized Hospital Specific Presentation on Quality, Safety, Compliance & Education
The Medicare Spending per Beneficiary MSPB measure is designed to assess the average spending per Medicare beneficiary, which is indicative of the efficiency and cost-effectiveness of a hospital or healthcare provider. By evaluating the total cost of services rendered during an MSPB episode, which includes the inpatient stay, 3 Days before the Inpatient Stay and the 30 days following discharge, CMS aims to identify variations in spending, incentivize cost reduction, and promote high-quality care.
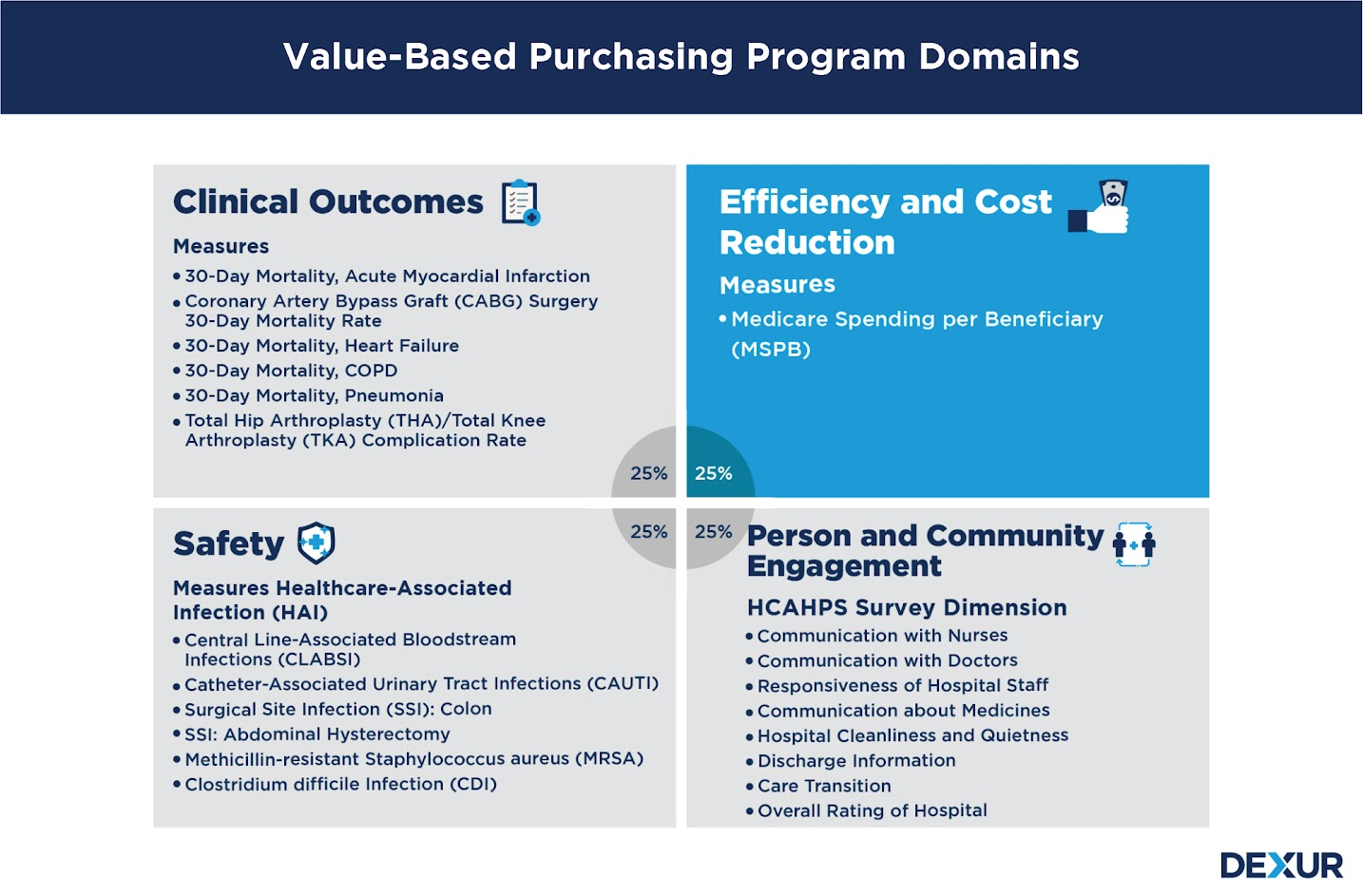
Why MSPB is Important for CMS Value Based Purchasing (VBP) Program
The Medicare Spending per Beneficiary (MSPB) measure holds substantial weight in calculating the total Value-Based Purchasing (VBP) domain score, constituting 25% of the overall score. The VBP program is a CMS initiative that rewards hospitals for providing high-quality, cost-effective care by adjusting payments based on their performance across various domains. The MSPB’s significant contribution to the total VBP domain score underscores the emphasis placed by CMS on cost-efficiency and resource utilization alongside clinical outcomes and patient experiences. This allocation of 25% signifies that hospitals need to strategically focus on managing costs during an MSPB episode to perform well in the VBP program and maximize their Medicare reimbursements, all while maintaining or improving the quality of patient care. Balancing cost and quality under the scrutiny of the MSPB measure thus becomes a pivotal aspect for healthcare providers participating in the VBP program.
MSPB Episode Length and Cost Calculation Methodology:

-
Defining MSPB Episode: An MSPB episode encompasses the inpatient stay, beginning three days before admission, and continuing for 30 days post-discharge, excluding unrelated costs.
-
Attribution of Episodes: Episodes are attributed to the hospital where the inpatient stay occurred, holding the institution accountable for the spending during the episode.
-
Risk Adjustment: The measure adjusts for factors such as beneficiary age, sex, comorbidities, and geographic variations to ensure fair comparisons.
-
Calculation of Hospital-Specific MSPB Amount: The MSPB amount for a specific hospital is calculated by comparing the hospital’s average spending per episode to the national median of spending per episode for all hospitals.
-
Normalization and Scoring: The measure is normalized to adjust for yearly changes, and hospitals are scored relative to the national median MSPB amount.
Exclusions in MSPB Methodology:
-
The beneficiary was not enrolled in Medicare Parts A and B for the entirety of the lookback period plus the episode window.
-
The beneficiary’s death occurred before the episode ended.
-
Any episode in which the index admission inpatient claim has a $0 actual payment.
-
Inpatient readmissions occurring in the 30-day post-discharge period of an episode are excluded from triggering new episodes.
-
Episodes where the beneficiary has a primary payer other than Medicare for any time during the episode window or 90-day lookback period prior to the episode start day.
What Types of Costs and Claims are Included in MSPB?
Each time frame within the episode length constitutes costs which include inpatients, outpatients, skilled nursing facility, home health, hospice, durable medical equipment, prosthetics, orthotics, and supplies, and Medicare Part B Carrier (non-institutional Physician/Supplier) claims. The costs refer to total allowed amounts as defined in Medicare claims data, which include Medicare institutional costs and beneficiary payments; as long as the start of the claim falls within the episode window of 3 days prior to the index admission through 30 days post-hospital discharge.
1. 3 Days Prior to Inpatient Stay:
In the three days leading up to the inpatient stay, several cost components are considered:
-
Home Health: Costs incurred for medical care provided at the beneficiary’s home to treat or manage a health condition.
-
Hospice: Expenses related to end-of-life care aimed at providing comfort and support to beneficiaries with terminal illnesses.
-
SNF (Skilled Nursing Facility): Charges for short-term rehabilitative services and nursing care needed before the inpatient admission.
-
Outpatient: Costs associated with outpatient hospital services and treatments received outside of inpatient hospitalization.
-
DME (Durable Medical Equipment): Expenses for medical equipment used at home that provides therapeutic benefits.
-
Carrier: Payments covering physician and clinical lab services that are billed independently.
2. During Index Hospital Stay:
The main cost component during this period is:
-
Inpatient Costs: These comprise all expenses associated with the beneficiary’s primary hospitalization, covering room charges, nursing, lab tests, medications, and any other services received during the stay.
3. 1 through 30 Days Post-Discharge:
Several cost components are analyzed post-discharge to understand the continuity of care and potential readmissions:
-
Home Health: Post-discharge home health costs represent the expenses for medical care, therapy, and assistance provided at the beneficiary’s home.
-
Hospice: If end-of-life care is initiated post-discharge, hospice costs are accounted for.
-
SNF: Costs for skilled nursing facilities are included if the beneficiary requires rehabilitative care and skilled nursing post-discharge.
-
Inpatient (Due to Readmissions): Any costs associated with readmissions to the hospital within 30 days post-discharge are accounted for, reflecting the quality of care and potential areas for improvement.
-
Outpatient: Expenses related to outpatient services, treatments, or consultations received after discharge are included.
Leveraging Dexur's Capabilities for MSPB Monitoring and Improvement
In a landscape where hospitals have restricted access to inpatient data, Dexur is an invaluable ally, offering insights into the entire patient journey, granular cost component simulations, and timely DRG and MDC level breakdowns.
1. Access to Comprehensive Medicare Claims Data
Dexur, as an approved purchaser of Medicare claims data, holds a unique position enabling it to access information across the entire spectrum of a patient’s healthcare journey. Unlike individual hospitals, which are limited to inpatient data, Dexur can monitor a patient’s interactions with various healthcare touchpoints, including Skilled Nursing Facilities (SNF), Home Health agencies, and other inpatient facilities. This comprehensive access allows for a more accurate and holistic analysis of MSPB, revealing hidden patterns and areas of potential improvement that would otherwise remain unnoticed.
2. Simulation of Post-Discharge Cost Components
Armed with a wealth of data, Dexur employs sophisticated simulation techniques to dissect and analyze each post-discharge cost component. Through these simulations, Dexur can project the impact of changes in individual cost components such as SNF, Readmission, and Home Health on the overall MSPB. For instance, Dexur's insights might reveal that a 20% reduction in SNF discharge rates or Readmission rates could lead to a 10% reduction in MSPB. Such a reduction not only signifies considerable cost savings but can also translate to a significant increase in Value-Based Purchasing (VBP) payouts, benefiting the healthcare provider financially
3. Detailed DRG and MDC Level Breakdowns
Beyond simulations, Dexur delves deep into the intricacies of MSPB through detailed Diagnosis-Related Group (DRG) and Major Diagnostic Category (MDC) level breakdowns by cost component. These breakdowns enable healthcare providers to pinpoint specific areas within different diagnoses and categories contributing to elevated MSPB. Notably, Dexur’s ability to provide this detailed analysis much sooner than CMS's final report offers healthcare providers a head start in implementing strategic changes and improvements.
4. Comparing Post Acute Care Providers' Costs
Displaying post-acute provider costs by individual Home Health Agencies and Skilled Nursing Facilities (SNFs) is a pivotal strategy that offers multifaceted benefits to hospitals aiming to lower Medicare Spending per Beneficiary (MSPB) costs. This granular view into provider-specific costs enables hospitals to identify and collaborate with the most cost-effective and high-performing post-acute care providers,optimizing the entire patient care continuum. Hospitals can make informed and strategic decisions regarding patient referrals by understanding which Home Health agency or SNF has demonstrated the best performance in cost management and quality of care.This not only fosters a more seamless and efficient transition of care but also contributes significantly to the reduction of overall MSPB costs. In turn, this can enhance the hospital's standing in the Value-Based Purchasing program, leading to improved patient outcomes and potential financial rewards. Moreover, providing such transparency and insight fosters a competitive environment among post-acute care providers, encouraging them to elevate their standards of care and cost efficiency continually.
By leveraging the insights and analyses provided by Dexur, healthcare providers can formulate and execute data-driven strategies to optimize MSPB. The nuanced understanding of how alterations in individual cost components can affect MSPB allows for targeted interventions and resource allocation. Whether it’s reducing readmission rates, optimizing SNF discharges, or enhancing home health care, the actionable insights derived from Dexur’s analyses pave the way for measurable improvements in MSPB and, consequently, in VBP payouts.