How Clinical Peer Reviews Can Not Only Meet Accreditation Requirements but Also Drive Improvements in Quality Program Outcomes
Get Dexur’s Personalized Hospital Specific Presentation on Quality, Safety, Compliance & Education
Peer review is a critical component in the accreditation and quality assurance processes for healthcare organizations. The Joint Commission (TJC), the Centers for Medicare & Medicaid Services (CMS), Det Norske Veritas (DNV), and the National Committee for Quality Assurance (NCQA) each have specific expectations regarding peer review processes.
The Joint Commission (TJC)
TJC, a leading healthcare accreditation organization in the United States, integrates peer review into its standards to improve patient care quality and safety. TJC requires accredited healthcare organizations to have a defined process for peer review as part of their ongoing professional practice evaluation (OPPE) and focused professional practice evaluation (FPPE) standards. These processes are essential components of the credentialing and privileging procedures, enabling organizations to assess the competence of their practitioners systematically. Through OPPE and FPPE, TJC ensures that healthcare providers are evaluated on their clinical practice performance, incorporating peer review feedback to identify areas for improvement, support professional development, and, when necessary, take corrective action.
Centers for Medicare & Medicaid Services (CMS)
CMS, which oversees the Medicare and Medicaid programs, incorporates peer review in several aspects of healthcare delivery, including the Quality Improvement Organization (QIO) Program. Furthermore, peer review is integral to the Conditions of Participation (CoPs) for hospitals related to quality assurance and performance improvement (QAPI)., under which CMS requires hospitals to have established processes for credentialing and privileging, including the use of peer review data to assess provider performance. These CoPs necessitate that hospitals have a QAPI program that effectively monitors and improves the quality of healthcare provided. Within this framework, peer review plays a crucial role in identifying areas for clinical improvement, assessing practitioner performance, and implementing evidence-based practices to enhance care delivery and patient outcomes. Compliance with CMS CoPs is essential for hospitals to maintain their Medicare and Medicaid certification.
Det Norske Veritas (DNV)
DNV, an international accrediting body with a unique integration of ISO 9001 quality management system standards within healthcare accreditation, emphasizes the significance of peer review in maintaining clinical quality and safety. DNV's accreditation standards for hospitals include requirements for the implementation of a peer review process as part of the hospital's quality management system. This process is aimed at monitoring the performance of medical staff and identifying opportunities for improvement. DNV requires that peer review is conducted in a systematic, ongoing manner, contributing to the continuous improvement of healthcare services and compliance with DNV's healthcare standards.
National Committee for Quality Assurance (NCQA)
NCQA, primarily focused on the accreditation of health plans and the certification of various healthcare organizations, incorporates peer review in its standards, particularly in the context of credentialing. NCQA's standards require health plans to conduct credentialing reviews of their providers, which includes the use of peer review information to assess providers' clinical competence and performance. This process ensures that providers contracted by health plans meet high-quality standards, ultimately aiming to improve the quality of care available to plan members.
The Missed Opportunity to Align Peer Review with Quality Programs
Despite the critical role peer review programs play in ensuring clinical excellence and adherence to healthcare standards, there exists a notable disconnect between these programs and broader quality improvement initiatives such as the CMS Star Rating, Hospital Readmission Reduction Program (HRRP), Value-Based Purchasing (VBP), The Leapfrog Group, and the Hospital-Acquired Condition Reduction Program (HACRP). This gap represents a missed opportunity for aligning frontline care practices with the metrics that significantly impact healthcare organizations' quality ratings and financial incentives.
Examples of Missed Opportunities
-
AMI Mortality and CMS Star Ratings: AMI mortality rates are a critical measure in the CMS Star Rating system. A peer review process that does not specifically focus on reviewing care provided to AMI patients, especially those that resulted in mortality, misses a crucial opportunity to improve performance on this measure.
-
COPD Readmissions and HRRP: COPD readmissions are a focus of the HRRP, aiming to reduce unnecessary readmissions for COPD patients. Peer reviews that do not concentrate on the care transitions and discharge planning for COPD patients may fail to address gaps that lead to readmissions, thus not supporting efforts to improve HRRP performance.
-
CLABSI and Quality Programs: Infections like CLABSI have a profound impact on a hospital's performance in various quality programs, including VBP, Leapfrog, and HACRP. Without a targeted peer review focus on the prevention, identification, and management of CLABSI cases, hospitals may not effectively address one of the key areas affecting their quality scores and financial penalties.
Disconnection Between Peer Review and Quality Programs
-
Focus on General Clinical Competence Over Specific Quality Measures: Peer review processes often concentrate on evaluating general clinical competence and adherence to standard care protocols. While this is crucial for ensuring that healthcare providers meet baseline quality and safety standards, it may overlook the specific measures that directly influence quality program outcomes. For instance, a peer review might assess overall care for patients with acute myocardial infarction (AMI) but not specifically focus on the aspects of care that affect AMI mortality rates, a key metric for the CMS Star Rating.
-
Lack of Integration with Key Quality Measure Data: Peer review programs might not systematically incorporate data on specific quality measures such as COPD readmissions, which affect HRRP outcomes, or central line-associated bloodstream infections (CLABSI), critical to most quality programs. Without explicitly reviewing cases or care practices linked to these measures, peer reviews may miss targeted opportunities for quality improvement.
-
Limited Alignment with Quality Improvement Goals: Although peer review is designed to enhance care quality, the lack of explicit alignment with the goals of quality programs can lead to disjointed improvement efforts. Quality programs focus on specific outcomes and metrics, such as readmission rates or infection rates, that directly impact hospital ratings and financial penalties or rewards. Without a clear strategy to align peer review focus areas with these metrics, the potential impact on improving specific quality program outcomes is diminished.
-
Missed Opportunities for Educating and Engaging Frontline Professionals: The disconnection between peer review and quality improvement initiatives represents a missed opportunity to engage frontline professionals in targeted quality improvement efforts. By not focusing peer reviews on the specific measures that affect quality ratings and financial incentives, healthcare organizations miss out on the chance to directly involve care providers in understanding and improving these key performance areas.
Bridging the Gap
To address this disconnection and fully leverage the potential of peer review programs to enhance quality program outcomes, healthcare organizations could consider the following strategies:
-
Integrate Quality Measure Data into Peer Review Processes: Explicitly include data on specific quality measures, such as those affecting CMS Star Ratings, HRRP, VBP, Leapfrog, and HACRP, in the peer review criteria. This integration would ensure that cases and practices directly impacting these measures are reviewed and addressed.
-
Align Peer Review Focus with Quality Improvement Objectives: Develop peer review protocols that specifically target areas of care impacting quality program metrics. For instance, focusing peer reviews on care practices related to high-risk conditions like AMI, COPD, or CLABSI can directly contribute to improving relevant quality measures.
-
Educate and Engage Frontline Professionals: Use peer review findings related to specific quality measures as educational tools for frontline professionals. Highlighting how specific care practices influence quality ratings and financial outcomes can motivate and guide improvements in clinical practice.
-
Continuous Monitoring and Feedback Loop: Establish a continuous monitoring system that feeds data from quality programs back into the peer review process. This approach ensures that peer review efforts remain aligned with evolving quality improvement goals and outcomes.
By addressing these disconnections and strategically aligning peer review programs with quality improvement initiatives, healthcare organizations can enhance their ability to deliver high-quality care, improve patient outcomes, and achieve better performance in key quality metrics and financial incentives.
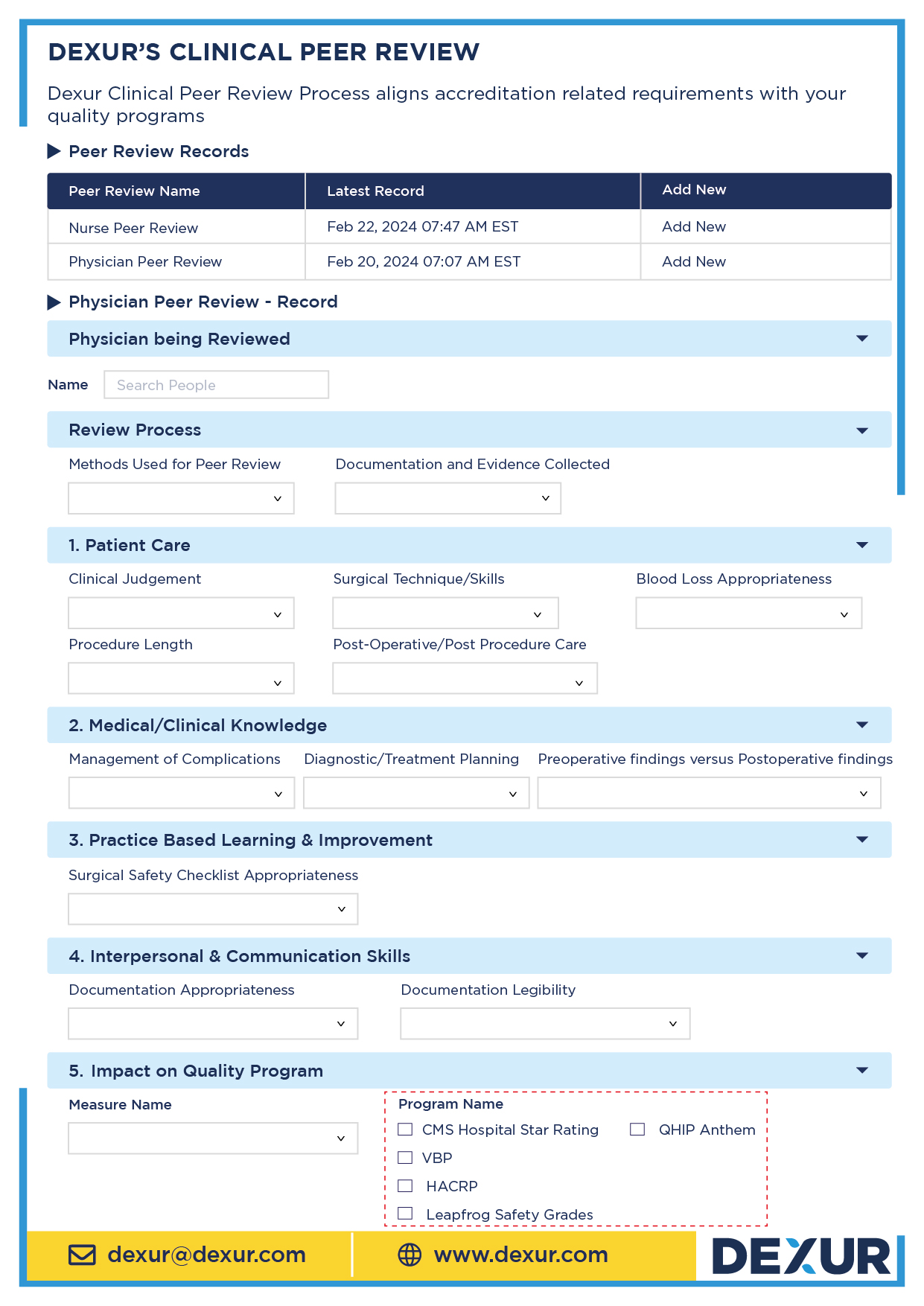
Connecting Accreditation Requirements with Quality Program Improvement through Dexur's Unified Software
Dexur's Unified Quality, Safety, Risk, Incident, and Peer Review software presents an innovative solution to bridging the gap between clinical peer review programs and quality improvement initiatives such as CMS Star Ratings, the Hospital Readmission Reduction Program (HRRP), Value-Based Purchasing (VBP), The Leapfrog Group assessments, and the Hospital-Acquired Condition Reduction Program (HACRP). By integrating accreditation requirements with actionable data insights, Dexur facilitates targeted improvements in healthcare delivery and patient outcomes. This section highlights how Dexur's software can transform the alignment of peer review processes with key quality measures, leveraging real-world examples.
Streamlining Focus on Key Quality Measures
Traditional peer review processes often operate in silos, focusing on individual provider performance and specific patient encounters without necessarily aligning with broader organizational quality goals. For instance, while peer reviews might evaluate general clinical competencies, they may overlook specific cases impacting critical quality measures like AMI mortality, COPD readmissions, or CLABSI infections. Dexur's software addresses this disconnect by integrating data analytics and peer review functionalities, ensuring that reviews are directly linked to measures affecting an organization's performance in quality programs.
Example: Targeted Peer Review for AMI Mortality
Using Dexur’s software, a hospital can identify that its AMI mortality rates are higher than national benchmarks, directly affecting its CMS Star Ratings. The software allows the hospital to specifically target peer reviews of AMI cases, correlating clinical practices with mortality outcomes. Through detailed analytics, the software highlights potential areas for clinical improvement, such as the timing of medication administration or adherence to evidence-based care protocols. This targeted approach ensures that peer reviews are not only comprehensive but also strategically focused on enhancing care areas critical to the hospital's quality performance.
Enhancing HRRP Performance through Data-Driven Insights
For hospitals struggling with high readmission rates for conditions like COPD, Dexur’s platform can systematically identify cases that resulted in readmissions within the 30-day post-discharge period. By conducting peer reviews focused on these cases, healthcare providers can uncover root causes, such as gaps in discharge planning or patient education. The software’s integration of risk, incident, and peer review data enables a holistic understanding of factors contributing to readmissions, facilitating targeted interventions to improve patient transitions and reduce readmissions.
Aligning with HACRP through Incident and Peer Review Correlation
Dexur’s unified platform excels in correlating incident reporting with peer review processes, particularly in the context of hospital-acquired infections like CLABSI. By analyzing incidents of CLABSI infections, the software enables healthcare organizations to focus peer reviews on infection prevention practices, adherence to sterile procedures, and the effectiveness of staff training programs. This approach not only aids in identifying specific areas for improvement but also aligns peer review efforts with critical HACRP measures, enhancing patient safety and reducing hospital-acquired conditions.
Dexur's Unified Quality, Safety, Risk, Incident, and Peer Review software offers a comprehensive solution to the often observed disconnect between clinical peer review programs and key quality improvement measures. By leveraging data analytics to guide peer review processes, Dexur ensures that healthcare organizations focus on areas with the most significant impact on quality ratings and patient outcomes. Through targeted reviews, actionable insights, and the integration of quality, safety, and risk data, Dexur empowers healthcare providers to align frontline care with overarching quality goals, ultimately advancing healthcare quality and patient safety.