A Deep Dive into CMS's Excess Days in Acute Care (EDAC) Methodology
Get Dexur’s Personalized Hospital Specific Presentation on Quality, Safety, Compliance & Education
The Centers for Medicare & Medicaid Services (CMS) developed the Excess Days in Acute Care (EDAC) methodology as a critical tool for assessing and managing healthcare efficiency, particularly in relation to post-discharge care. This methodology is a significant element in the CMS Star Rating system, especially in the Readmission Group, which carries a substantial weight of 22%. By evaluating excess days spent in acute care settings, EDAC offers insights into the effectiveness of hospital discharge planning and post-discharge care coordination.

How should hospitals interpret and use the EDAC measures?
Hospitals interpret EDAC measures to gauge acute care use post-hospitalization for AMI, HF, and pneumonia. Effective care transitions, like appropriate discharge locations, clinician communication, accurate medication reconciliation, and timely follow-ups, reduce the likelihood of ED visits, observation stays, or readmissions within 30 days after discharge. Improved processes often result in fewer or shorter returns to acute care. EDAC results can be negative, zero, or positive.
| EDAC Result | Interpretation |
|---|---|
| Negative EDAC | Indicates your patients spent fewer days in acute care than would be expected if admitted to an average performing hospital with your case mix. |
| An EDAC of zero | Indicates your hospital is performing exactly as expected. |
| Positive EDAC | Indicates your patients spent more days in acute care than would be expected if admitted to an average performing hospital with your case mix. |
Inclusion Criteria Expanded:
-
Patients must be aged 65 years or older.They should be enrolled in both Part A and Part B of Medicare Fee-for-Service (FFS) for the 12 months leading up to the admission date. Additionally, they must be enrolled in Part A during the index admission
-
Discharge Setting: Patients must be discharged alive and should not have been transferred to another acute care facility.
-
Principal Discharge Diagnosis: Includes patients with specific diagnoses such as Acute Myocardial Infarction (AMI), Heart Failure (HF), and Pneumonia (PN), which are common and significant causes of hospital readmissions.
Exclusion Criteria Detailed:
-
Excludes cases where patients were discharged against medical advice (AMA) due to not receiving the full course of treatment.
-
Planned diagnosis/procedure codes listed in the AMI/HF/PN Supplemental file should be excluded.
-
Critical access hospitals, behavioral health, and psychiatric hospitals are not considered in this context.
EDAC Methodology
-
The outcome for the AMI, HF, and PN EDAC measures summarizes the time that patients spent in the ED, observation stays, and unplanned inpatient readmission for any reason within 30 days after discharge from an eligible index admission.
Outcome Calculation:
-
Emergency Department (ED) visits are partially counted (0.5 days), reflecting their role in acute care but recognizing their limited scope compared to full hospitalization. If a patient visits the ED once, this is counted as 0.5 days (regardless of how long the patient spends in the ED). If a patient visits the ED twice, this is counted as 1 day.
-
Observation stays, often a gray area between outpatient and inpatient care, are quantified in a standardized manner. If a patient spends 3 hours in observation, this is counted as 0.5 days. If a patient spends 17 hours In observation, this is counted as 1 day.
-
Unplanned readmissions, a key indicator of potential gaps in care, are measured based on the length of stay to reflect the severity of the readmission. If a patient spends 0.5 calendar days in readmission, this is counted as 1 day. If a patient is admitted on the first day of the month and discharged on the 10th day of the month, this is counted as 9 days.
Performance Calculation:
-
The comparison between predicted and expected days offers a nuanced view of hospital performance, adjusting for the complexity of cases handled by each hospital.
-
This methodology enables a fair assessment by comparing hospitals with a similar case mix, thus controlling for factors like patient demographics and baseline health status.
This comprehensive approach by CMS aims to encourage hospitals to improve discharge planning and post-discharge care coordination, ultimately reducing unnecessary readmissions and enhancing patient care outcomes.
Overlapping EDAC Outcome Events
While calculating the Excess Days Acute Care (EDAC) measures, when eligible acute care events such as an ED (Emergency Department) visit, observation stay, or unplanned inpatient readmission occur on the same day and overlap, the EDAC measures count only the time spent in the most severe of the overlapping events. The order of severity for the EDAC outcome events, from least to most severe, is as follows:
-
Emergency Department (ED) Visit: An Emergency Department visit is typically considered the least severe of the three events. It involves a patient seeking emergency medical care at the hospital's emergency department. ED visits are generally shorter in duration compared to observation stays or inpatient readmissions.
-
Observation Stay: Observation stays are the next level of severity in the hierarchy. During an observation stay, a patient is admitted to the hospital for a period of time to receive additional medical care or monitoring that cannot be provided in the ED. Observation stays are usually longer in duration than ED visits but shorter than inpatient readmissions.
-
Unplanned Inpatient Readmission: Unplanned inpatient readmission is the most severe event in the EDAC context. It occurs when a patient, who has previously been discharged from the hospital, returns due to a medical condition that requires inpatient care. Inpatient readmissions typically involve an extended hospital stay and are considered the most resource-intensive.
High EDAC often correlates with lower patient outcomes and satisfaction, influencing the overall quality score and CMS Star rating negatively.
How can Dexur helps?
Dexur's Unified Quality, Safety, Risk, and Incident Management Software, with its AI-driven insights and cost-efficient, offers an integrated solution for EDAC challenges in hospitals, platform that assists hospitals and healthcare facilities in tracking and managing EDAC (Excess Days in Acute Care) across three main components: Unplanned Readmission Excess Days, Observation Stays Excess Days, and ER (Emergency Room) Excess Days. It provides access to historical data, trend analysis, and benchmarking capabilities to help healthcare providers identify areas for improvement in patient care, optimize patient flow, and reduce excessive stays in observation and ER post-discharge. Dexur's platform empowers healthcare organizations to make data-driven decisions and enhance both the quality and efficiency of their services.
AI-Driven Predictive Analysis:
Dexur AI utilizes the latest CMS medicare data to analyze healthcare trends, providing predictive insights like pinpointing elements that lead to patient readmissions.This predictive capability assists hospitals in strategic planning and decision-making. Hospitals can effectively track their progress and fine-tune their approaches, ensuring they are continually moving towards enhanced quality and patient care outcomes.

The chart provides a detailed breakdown of a sample hospital's (Acme Hospital) Excess Days in Acute Care (EDAC) for Acute Myocardial Infarction (AMI), Heart Failure (HF), and Pneumonia (PN).
EDAC is a critical component of the Readmission Group, which eventually contributes to the CMS Star Rating Program. These rates are used to evaluate the quality of care a hospital provides, with lower EDAC rates suggesting better care and outcomes. Hospitals are tasked with improving these rates to enhance patient outcomes and reduce the financial burden associated with readmissions. This is where Dexur's platform becomes instrumental.
Dexur Identifies Key Measures for Acme Hospital’s Improvement in CMS Star Ratings:
-
Excess Days - AMI (EDAC_30_AMI): This measure needs to Decrease AMI Excess Days (EDAC_30_AMI) from 37.2 (10th Percentile) to 15.0 (30th Percentile).
-
Excess Days - HF (EDAC_30_HF): This measure needs to Decrease Heart Failure Excess Days (EDAC_30_HF) from 50.5 (10th Percentile) to 16.0 (30th Percentile).
-
Excess Days - PN (EDAC_30_PN): This measure needs to Decrease Pneumonia Excess Days (EDAC_30_PN) Readmission from 47.9 (10th Percentile) to 16.2 (30th Percentile).
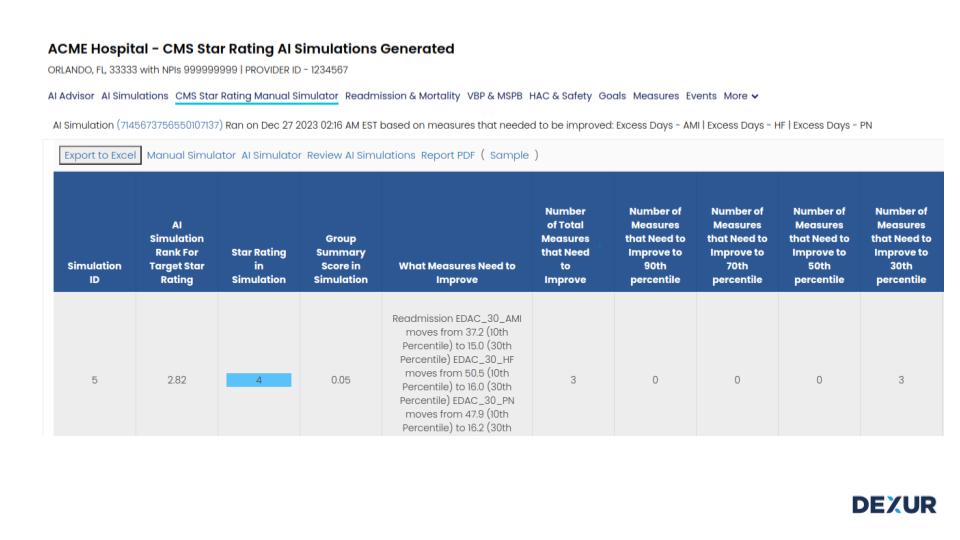
The table indicates that Acme Hospital must focus on enhancing these three specific Readmission measures to progress from 3-Star to 4-Star in the CMS Star Rating.

The bar chart presents a comparison of Acme Hospital’s Excess Days in Acute Care (EDAC) for Acute Myocardial Infarction (AMI) against the National Dexur Score for FY 2025 and FY 2026. Acme Hospital has more excess days in acute care for AMI patients compared to the National benchmark for the years 2025 and 2026 (as forecasted by Dexur) implying the scope for improvement in Readmission EDAC measures.
The table also demonstrates Unplanned Readmission Excess Days, ER Excess Days, and Observation Stays Excess Days that constitute the EDAC rate. Dexur's data for Acme Hospital, spanning from 2025 to a forecasted 2026, highlights how minor variations in readmission numbers can significantly impact the overall EDAC measure score. Additionally, Dexur’s AI meticulously analyzes CMS data, thereby gaining insights into prevailing trends. This sophisticated approach enables Dexur to accurately forecast future trends (2025 & 2026 FY Data) with a remarkable 98% accuracy in predictions. This predictive capacity sheds light on potential future scenarios and empowers healthcare providers like Acme Hospital with the foresight needed for effective planning and decision-making in healthcare management.
Realistic and Attainable Goal Setting:
Dexur's AI Advisor and analytics platform offer healthcare providers powerful tools to make data-driven decisions, set strategic goals, and track the effectiveness of their interventions. This approach is crucial for hospitals aiming to improve their performance in a competitive healthcare landscape.
-
CMS Star Rating Simulations: Dexur's simulations demonstrate how slight enhancements in various measures can elevate a hospital's ranking and positively affect their Group Summary Score. Hospitals can use these simulations to explore different scenarios and understand how changes in each measure group impact their overall Star Rating.
-
Setting Strategic Goals: Given the narrow performance range, hospitals need to continually strive for improvement. A slight decline in performance can significantly affect Star Ratings and other quality measures. Dexur's analytics platform assists healthcare providers in setting strategic, data-informed goals based on their simulations and priorities.
-
Tracking and Evaluating Interventions: With tight performance percentiles, it's challenging to discern the effectiveness of interventions. Dexur’s platform enables hospitals to track events and interventions, providing quantifiable data on their impact on performance measures.
Dexur supports hospitals in setting a variety of practical goals related to readmission rates. By clearly defining targets for care during a hospital stay and after discharge, hospitals can set specific, data-driven goals.

The bar chart presents Dexur AI's Advisory outcomes for Acme Hospital's target AMI Readmission rates at the 50th, 70th, and 90th percentiles. It shows the observed rates of Acute Myocardial Infarction (AMI) 30-day Readmissions across various intervals, aligned with CMS Star Rating timelines, from 2022 to 2026. These rates have a noticeable increase over time, suggesting a need for strategic improvement.
Marked by three red horizontal lines, the 50th, 70th, and 90th percentiles act as national benchmark standards for AMI readmissions, offering a gauge for the hospital's performance relative to nationwide data. These benchmarks underline the necessity for Acme Hospital to set specific goals in the measures, such as the 3 Day Post Discharge check-in and support for high-risk patients, to achieve their objectives for a higher CMS Star Rating percentile.
For the 2026 CMS Star Rating, Acme Hospital needs to reduce its AMI Readmissions rates from 18.95% to 13.9% to get a position in the 90th Percentile or 5-Star CMS Rating.
Dexur’s Incident Management Forms:
Hospitals seeking to optimize management and reduce unnecessary acute care days for patients with Pneumonia, Heart Failure, or Acute Myocardial Infarction (AMI) can achieve this through Dexur’sIncident Management Forms. This platform enhances patient care management by facilitating precise and efficient data collection tailored to each patient's specific needs and challenges, using Dexur's Incident reporting forms.

Figure- Dexur Incident Reporting Form
These data-driven insights, obtained by concentrating on particular readmission cases, empower healthcare providers to implement more targeted interventions. This approach
fosters an ongoing and comprehensive enhancement in patient care outcomes.
Dexur's Unified Quality, Safety, Risk, and Incident Management Software is a pivotal tool for hospitals aiming to improve their CMS Star Rating. The strategic approach of setting realistic goals and leveraging the AI Advisory Insights aligned with CMS compliance helps hospitals achieve higher CMS Star Ratings, reflecting their commitment to excellence in healthcare delivery.