Medicare Spending per Beneficiary (MSPB): Dexur Methodology, Calculations, and Importance
Get Dexur’s Personalized Hospital Specific Presentation on Quality, Safety, Compliance & Education
Importance of MSPB and other VBP Measures
Dexur analyzes Medicare Claims data to evaluate MSPB cost per episode for hospitals. MSPB Hospital measure assesses the cost to Medicare for services performed by hospitals and other healthcare providers during an episode of care (episode), which is composed of the periods immediately prior to, during, and following a patient’s hospital stay. CMS stresses the importance of measuring the cost of care explicitly to recognize hospitals that are involved in the provision of high-quality care at a lower cost, in conjunction with other quality measures.
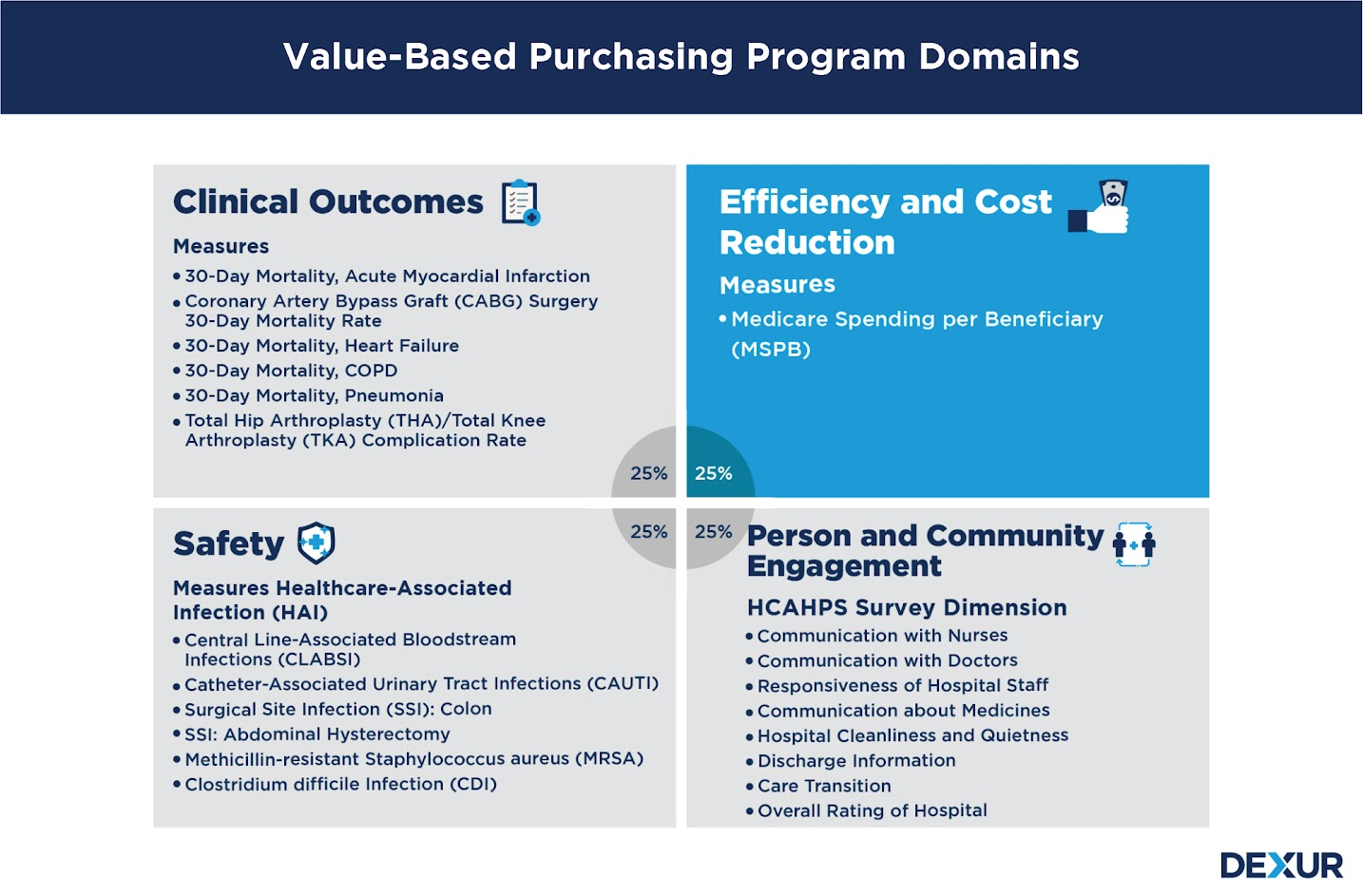
The Hospital VBP Program is designed to improve the quality, efficiency, and safety of care that patients receive during acute care inpatient stays, as well as to improve their experience of care during hospital stays. CMS evaluates hospital performance on an approved set of measures and dimensions grouped into four specific quality domains: clinical outcomes, efficiency and cost reduction, safety, and person and community engagement. Domains are assigned equal weights (percentages) of the Total Performance Score.
MSPB: Dexur Methodology
In order to calculate the Medicare spending per beneficiary for each hospital, we determined the following:
- The time frame, or length of the ‘‘spending per beneficiary episode’’ during which Medicare payments would be aggregated.
- The types of Medicare payments to be aggregated over this time frame.
MSPB Episode Length and Cost Calculations
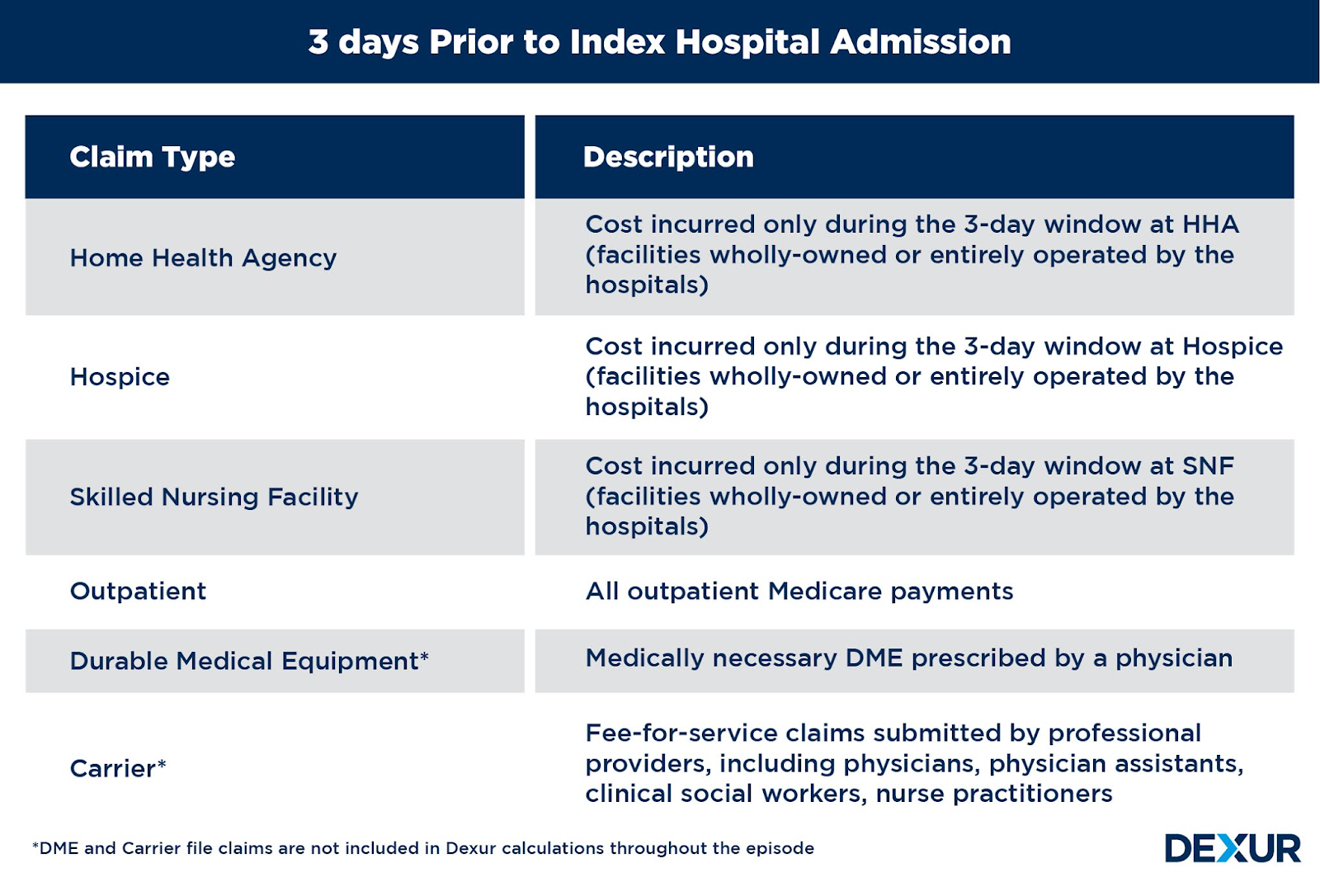
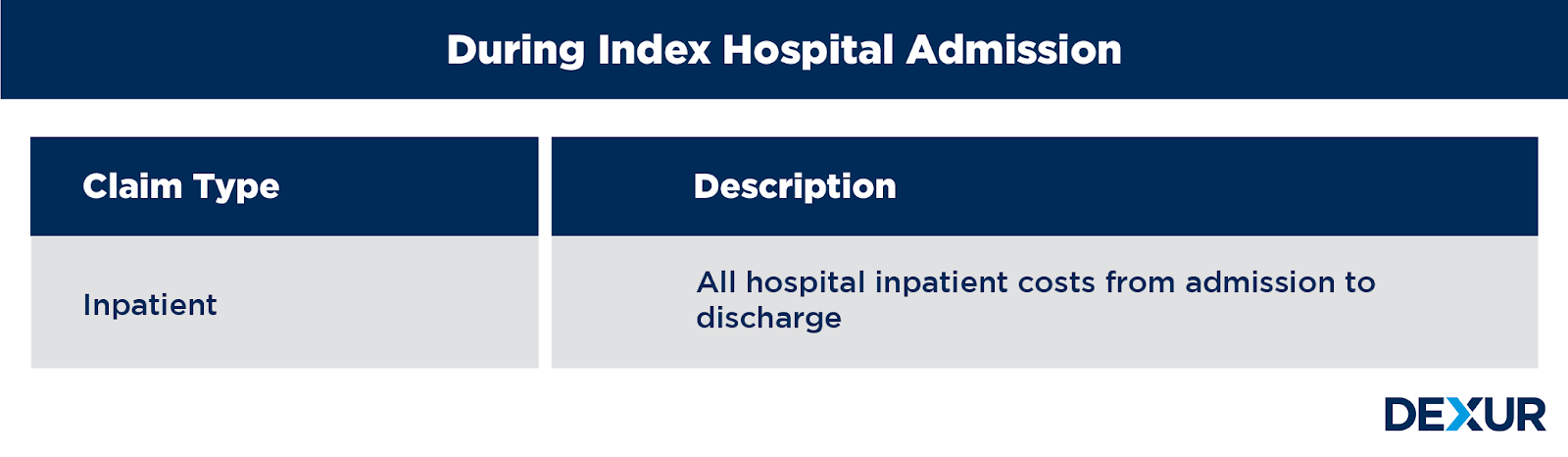
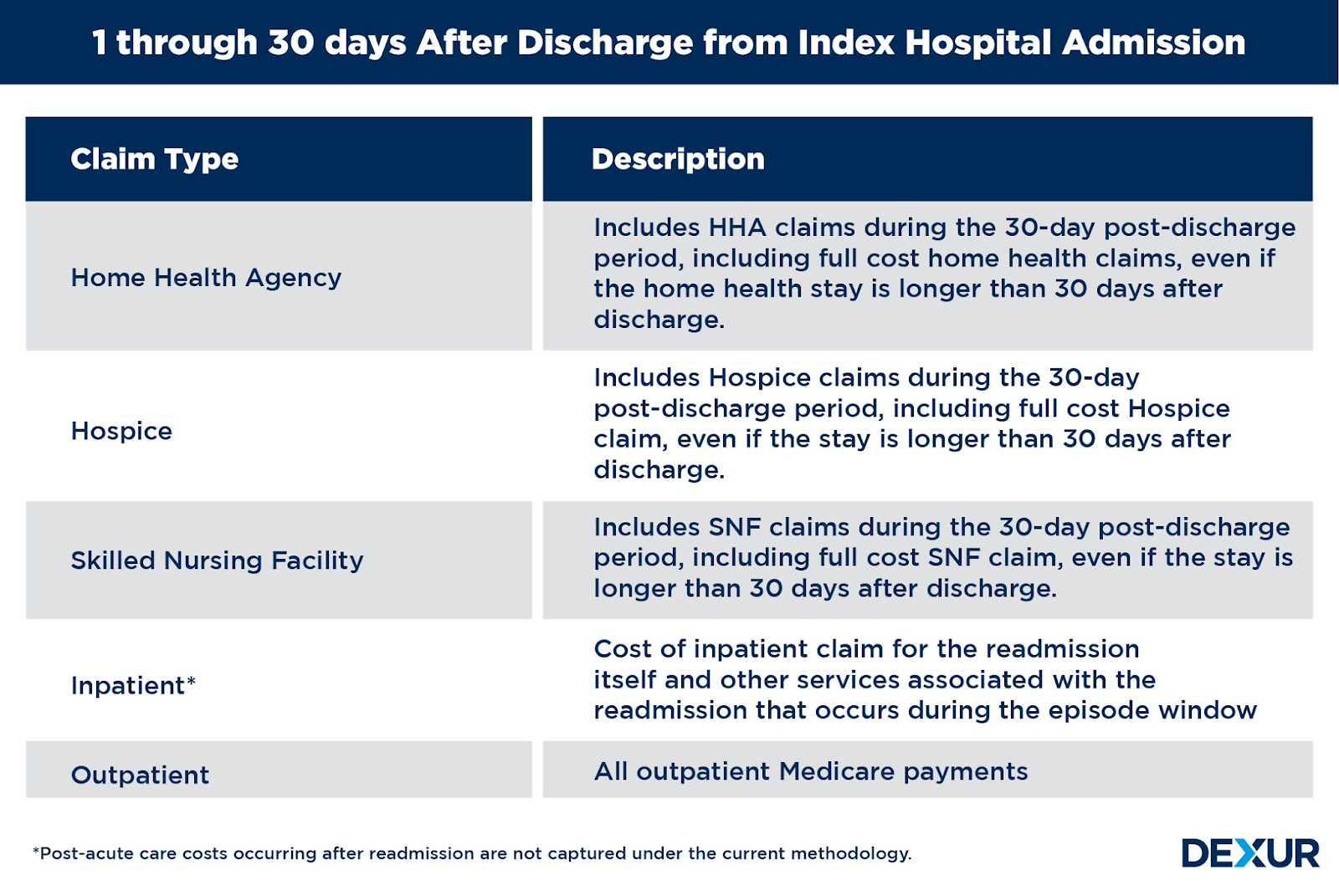
Medicare Part A and B costs are measured from the 3 days prior to inpatient hospitalization, during inpatient hospitalization, and 30 days after discharge from the hospital. An acute care hospital admission triggers the MSPB Hospital measure episode. Episodes are considered only for beneficiaries who have enrolled in Medicare Part A and Part B for the period 90 days prior to the start of an episode (i.e., 93 days prior to the date of the index admission) until 30 days after discharge.

Exclusions:
- The beneficiary was not enrolled in Medicare Parts A and B for the entirety of the lookback period plus episode window.
- The beneficiary’s death occurred before the episode ended.
- Any episode in which the index admission inpatient claim has a $0 actual payment.
- Inpatient readmissions occurring in the 30-day post-discharge period of an episode are excluded from triggering new episodes.
- Episodes where the beneficiary has a primary payer other than Medicare for any time during the episode window or 90-day lookback period prior to the episode start day.
How Dexur’s MSPB calculations are different from CMS’?
- CMS provides MSPB scores that evaluate hospitals’ costs compared to the national median (or midpoint) hospital costs. Dexur calculates average spending levels during hospitals’ MSPB episodes by Medicare claim type.
- Dexur breaks down the average spending in 3 time periods, which are further broken down into multiple claim types at the DRG level. CMS publishes similar data but provides overall hospital averages.
- Beneficiaries whose primary insurance becomes Medicaid during an episode due to exhaustion of Medicare Part A benefits, are included in the calculation.
- Psychiatric hospitals, rehabilitation hospitals and hospitals involved extensively in treatment for or research on cancer, are included to initiate episodes.
- DME and Carrier file claims are not included throughout the episode.
Claim Types in each time period
Each time frame within the episode length constitutes costs which include inpatients, outpatients, skilled nursing facility, home health, hospice, durable medical equipment, prosthetics, orthotics, and supplies, and Medicare Part B Carrier (non-institutional Physician/Supplier) claims. The costs refer to total allowed amounts as defined in Medicare claims data, which include Medicare institutional costs and beneficiary payments; as long as the start of the claim falls within the episode window of 3 days prior to the index admission through 30 days post-hospital discharge.