Get Dexur’s Personalized Hospital Specific Presentation on Quality, Safety, Compliance & Education
This white paper is part of the Dexur Quality Sights education program which is focused on Hospital Quality and Safety topics and is read by CMOs, CNOs, CQOs, and Quality and Safety Teams. Please email dexurqualitysights@dexur5.com to request more white papers like this and receive updates from Dexur on quality and safety topics (not more than once per week)
Dexur White Papers & Posters Page
To see our previously published posters, click on this link
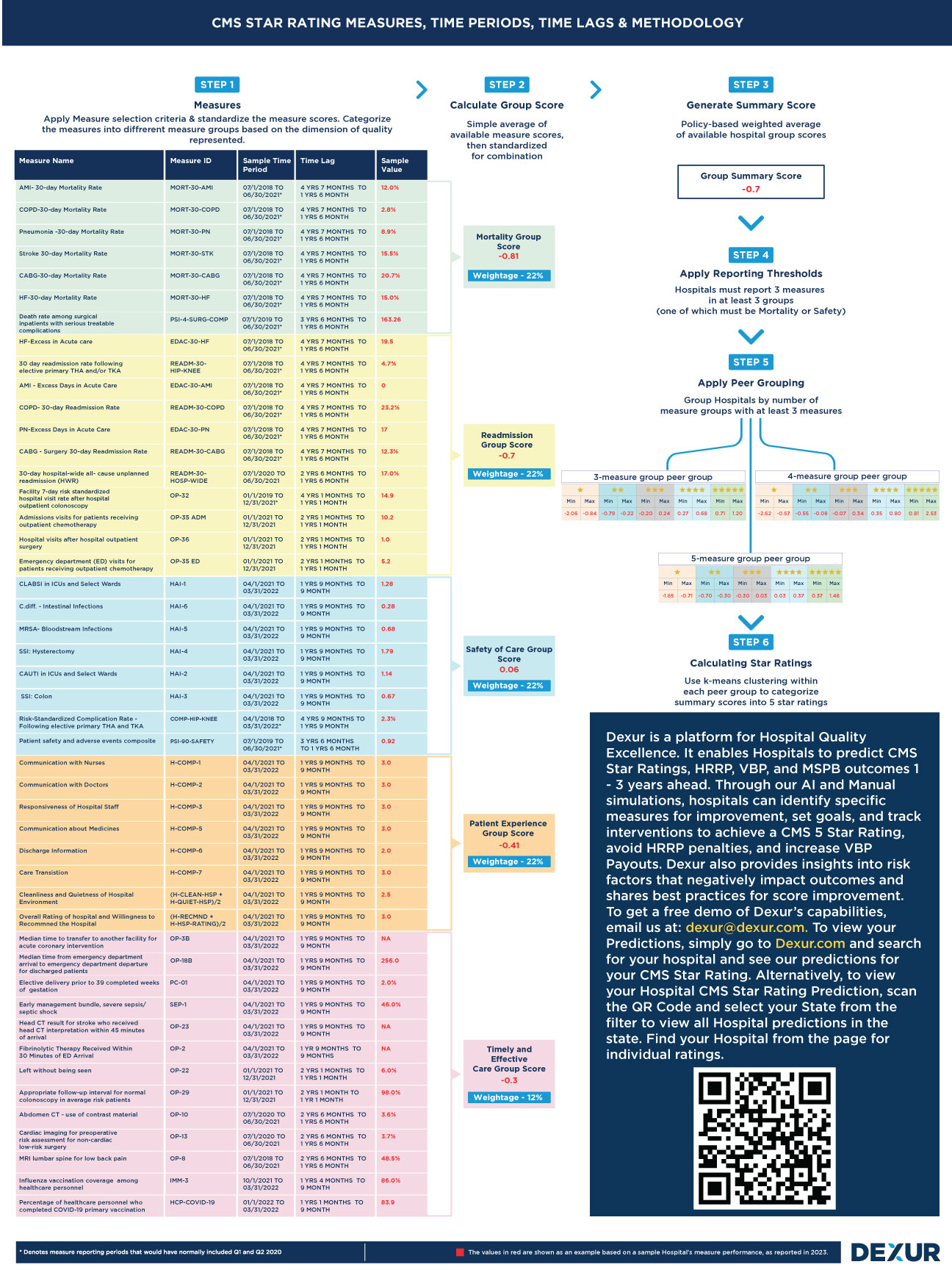
As part of educating, the quality community, Dexur is delighted to announce the release of a free poster, which meticulously consolidates all quality measures across various healthcare quality programs: CMS Star Rating, CMS Value-Based Purchasing (VBP), CMS Hospital-Acquired Condition Reduction Program (HACRP), CMS Hospital Readmissions Reduction Program (HRRP), and the Leapfrog Hospital Safety Grade.
Read moreDexur’s Free CMS Star Rating Measures, Time Periods, Time Lags and Methodology Poster
The Hospital CMS Star Ratings, designed to measure the quality of healthcare institutions, often presents hospitals with the challenging task of comprehending its intricate methodologies, encompassing performance periods, time lags, and specific weightages of different measures. Dexur, recognizing the complexity of these ratings, has identified that a significant portion of their interactions with hospitals revolves around elucidating these aspects. The need for clarity becomes particularly pronounced when considering that various teams within hospitals - from top-tier executives like the CEO, COO, CMO, CQO, and CNO to the Quality Departments - often have divergent understandings of how the Star Ratings function.
Read moreHow Dexur Helps Hospitals Achieve Quality Excellence
Hospitals are often surprised by the outcomes of CMS Programs and struggle to improve CMS Star Ratings and Payouts and reduce Penalties. This is because of four reasons:
- Lack of out-of-hospital data (e.g., for 30-day readmissions and mortality)
- Lack of expert resources to update changing quality measure algorithms
- Little room for error in final measure scores
- Lack of scale and budget to invest in modern software.