All The Hospital CMS Measures that Impact Star Rating, VBP, HRRP & HAC Programs
Get Dexur’s Personalized Hospital Specific Presentation on Quality, Safety, Compliance & Education
All CMS Measures at a Glance
CMS has come up with different programs to improve health outcomes by focusing on improving various aspects of the healthcare system. Dexur’s data provides in-depth information on the metrics of different programs such as CMS Star Ratings, VBP, HRRP, and HAC. While hospitals have to wait for more than a year to get this data from CMS, Dexur replicates CMS algorithms and updates the data at DRG levels only with a 5-6 month delay.
| All CMS Measures at a Glance | |||||||
|---|---|---|---|---|---|---|---|
| Measure Category | Measure Name | Measure Description | CMS Category | CMS Star Rating | Value-Based Purchasing (VBP) | Hospital Readmissions Reduction Program (HRRP) | Hospital-Acquired Condition (HAC) Reduction Program |
| Cost Effectiveness | MSPB | Medicare Spending Per Beneficiary | ⊜ | ||||
| Readmissions | READM-30-AMI | AMI- 30-day Readmission Rate | ⇄ | ||||
| Readmissions | READM-30-HF | Heart Failure- 30-day Readmission Rate | ⇄ | ||||
| Readmissions | READM-30-PN | Pneumonia- 30-day Readmission Rate | ⇄ | ||||
| Readmissions | READM-30-CABG | CABG - Surgery 30-day Readmission Rate | Readmission | ✰ | ⇄ | ||
| Readmissions | READM-30-COPD | COPD- 30-day Readmission Rate | Readmission | ✰ | ⇄ | ||
| Readmissions | READM-30-Hip-Knee | 30-day readmission rate following elective primary THA and/or TKA | Readmission | ✰ | ⇄ | ||
| Readmissions | READM-30-HOSP-WIDE | 30-day hospital-wide all- cause unplanned readmission (HWR) | Readmission | ✰ | |||
| Readmissions | READM-30-STK (2019) | Stroke -30-Day Readmission Rate | Readmission | ✰ (Included in FY2019 and Excluded in FY2017, FY2020, FY2021) |
|||
| Readmissions | EDAC-30-AMI | AMI - Excess Days in Acute Care | Readmission | ✰ | |||
| Readmissions | EDAC-30-HF | HF - Excess Days in Acute Care | Readmission | ✰ | |||
| Readmissions | EDAC-30-PN | PN - Excess Days in Acute Care | Readmission | ✰ | |||
| Readmissions | OP-32 | Facility 7-day risk standardized hospital visit rate after outpatient colonoscopy | Readmission | ✰ | |||
| Mortality | MORT-30-AMI | AMI- 30-day Mortality Rate | Mortality | ✰ | ⊜ | ||
| Mortality | MORT-30-HF | HF-30-day Mortality Rate | Mortality | ✰ | ⊜ | ||
| Mortality | MORT-30-PN | PN-30-day Mortality Rate | Mortality | ✰ | ⊜ | ||
| Mortality | MORT-30-CABG | CABG-30-day Mortality Rate | Mortality | ✰ | ⊜ (Included in FY2022, FY2023, FY2024 and Excluded in FY2020, FY2021) |
||
| Mortality | MORT-30-COPD | COPD-30-day Mortality Rate | Mortality | ✰ | ⊜ (Included in FY2021, FY2022, FY2023, FY2024 and Excluded in FY2020) |
||
| Mortality | MORT-30-STK | Stroke 30-day Mortality Rate | Mortality | ✰ | |||
| Mortality | PSI-4-SURG-COMP | Death rate among surgical inpatients with serious treatable complications | Mortality | ✰ | |||
| HAI/ HAC / Complications /Safety | COMP-HIP-KNEE | Risk-Standardized Complication Rate - Following elective primary THA and TKA | Safety of Care | ✰ | ⊜ | ||
| HAI/ HAC / Complications /Safety | HAI-1 (CLABSI) | CLABSI in ICUs and Select Wards | Safety of Care | ✰ | ⊜ | ⊕ | |
| HAI/ HAC / Complications /Safety | HAI-2 (CAUTI) | CAUTI in ICUs and Select Wards | Safety of Care | ✰ | ⊜ | ⊕ | |
| HAI/ HAC / Complications /Safety | HAI-3 (SSI - Colon) | SSI: Colon | Safety of Care | ✰ | ⊜ | ⊕ | |
| HAI/ HAC / Complications /Safety | HAI-4 (SI - Hysterectomy) | SSI: Hysterectomy | Safety of Care | ✰ | ⊜ | ⊕ | |
| HAI/ HAC / Complications /Safety | HAI-5 (MRSA) | MRSA - Bloodstream Infections | Safety of Care | ✰ | ⊜ | ⊕ | |
| HAI/ HAC / Complications /Safety | HAI-6 (C. Diff) | C.diff. - Intestinal Infections | Safety of Care | ✰ | ⊜ | ⊕ | |
| HAI/ HAC / Complications /Safety | PSI-90-Safety | Patient safety and adverse events composite | Safety of Care | ✰ | ⊜ (Included in FY2023, FY2024 and Excluded in FY2020, FY2021, FY2022) |
⊕ | |
| HCAHPS | H-CLEAN-HSP | Cleanliness of Hospital Environment | Patient Experience | ✰ | ⊜ | ||
| HCAHPS | H-COMP-1 | Communication with Nurses | Patient Experience | ✰ | ⊜ | ||
| HCAHPS | H-COMP-2 | Communication with Doctors | Patient Experience | ✰ | ⊜ | ||
| HCAHPS | H-COMP-3 | Responsiveness of Hospital Staff | Patient Experience | ✰ | ⊜ | ||
| HCAHPS | H-COMP-5 | Communication about Medicines | Patient Experience | ✰ | ⊜ | ||
| HCAHPS | H-COMP-6 | Discharge Information | Patient Experience | ✰ | ⊜ | ||
| HCAHPS | H-HSP-RATING | Overall Rating of Hospital | Patient Experience | ✰ | ⊜ | ||
| HCAHPS | H-QUIET-HSP | Quietness of Hospital Environment | Patient Experience | ✰ | ⊜ | ||
| HCAHPS | H-RECMND | Willingness to Recommend the Hospital | Patient Experience | ✰ | ⊜ | ||
| HCAHPS | H-COMP-7 | Care Transition | Patient Experience | ✰ | ⊜ | ||
| Effectiveness of Care | IMM-2 | Influenza immunization | Effectiveness of Care | ✰ (Included in FY2017, FY2019, FY2020 and Excluded in FY2021) |
|||
| Effectiveness of Care | IMM-3 | Influenza vaccination coverage among healthcare personnel | Effectiveness of Care | ✰ (Included in FY2017, FY2019, FY2020 and Excluded in FY2021) |
|||
| Effectiveness of Care | OP-22 | Left without being seen | Effectiveness of Care | ✰ | |||
| Effectiveness of Care | OP-23 | Head CT scan results for acute ischemic stroke or hemorrhagic stroke who received head CT scan interpretation within 45 minutes of arrival | Effectiveness of Care | ✰ | |||
| Effectiveness of Care | OP-29 | Appropriate follow-up interval for normal colonoscopy in average risk patients | Effectiveness of Care | ✰ | |||
| Effectiveness of Care | OP-30 | Colonoscopy interval for patients with a history of adenomatous polyps - avoidance of inappropriate use | Effectiveness of Care | ✰ (Included in FY2017, FY2019, FY2020 and Excluded in FY2021) |
|||
| Effectiveness of Care | OP-33 | External beam radiotherapy for bone metastases | Effectiveness of Care | ✰ | |||
| Effectiveness of Care | PC-01 | Elective delivery prior to 39 completed weeks of gestation | Effectiveness of Care | ✰ | |||
| Effectiveness of Care | SEP-1 | Early management bundle, severe sepsis/septic shock | Effectiveness of Care | ✰ | |||
| Effectiveness of Care | VTE-6 | Hospital acquired potentially preventable venous thromboembolism | Effectiveness of Care | ✰ (Included in FY2017, FY2019, FY2020 and Excluded in FY2021) |
|||
| Effectiveness of Care | OP-4 (2019) | Aspirin at Arrival | Effectiveness of Care | ✰ (Included in FY2019 and Excluded in FY2017, FY2020, FY2021) |
|||
| Timeliness of Care | ED-1b | Average (median) time patients spent in the emergency department, before they were admitted to the hospital as an inpatient A lower number of minutes is better | Timeliness of Care | ✰ (Included in FY2017, FY2019, FY2020 and Excluded in FY2021) |
|||
| Timeliness of Care | ED-2b | Median time from admit decision to time of departure from the emergency department for patients admitted to inpatient status | Timeliness of Care | ✰ | |||
| Timeliness of Care | OP-2 | Fibrinolytic therapy received within 30 minutes of emergency department arrival | Timeliness of Care | ✰ | |||
| Timeliness of Care | OP-3b | Median time to transfer to another facility for acute coronary intervention | Timeliness of Care | ✰ | |||
| Timeliness of Care | OP-5 | Median Time to ECG | Timeliness of Care | ✰ (Included in FY2017, FY2019, FY2020 and Excluded in FY2021) |
|||
| Timeliness of Care | OP-18b | Median time from emergency department arrival to emergency department departure for discharged patients | Timeliness of Care | ✰ | |||
| Timeliness of Care | OP-1 (2019) | Median Time to Fibrinolysis | Timeliness of Care | ✰ (Included in FY2019 and Excluded in FY2017, FY2020, FY2021) |
|||
| Timeliness of Care | OP-20 (2019) | Door to Diagnostic Evaluation by a Qualified Medical Professional | Timeliness of Care | ✰ (Included in FY2019 and Excluded in FY2017, FY2020, FY2021) |
|||
| Timeliness of Care | OP-21 (2019) | Median Time to Pain Management for Long Bone Fracture | Timeliness of Care | ✰ (Included in FY2019 and Excluded in FY2017, FY2020, FY2021) |
|||
| Efficient Use of Medical Imaging | OP-8 | MRI lumbar spine for low back pain | Efficient Use of Medical Imaging | ✰ | |||
| Efficient Use of Medical Imaging | OP-10 | Abdomen CT - use of contrast material | Efficient Use of Medical Imaging | ✰ | |||
| Efficient Use of Medical Imaging | OP-11 | Thorax CT Use of Contrast Material | Efficient Use of Medical Imaging | ✰ (Included in FY2017, FY2019, FY2020 and Excluded in FY2021) |
|||
| Efficient Use of Medical Imaging | OP-13 | Cardiac imaging for preoperative risk assessment for non-cardiac low-risk surgery | Efficient Use of Medical Imaging | ✰ | |||
| Efficient Use of Medical Imaging | OP-14 | Outpatients with brain CT scans who got a sinus CT scan at the same time | Efficient Use of Medical Imaging | ✰ (Included in FY2017, FY2019, FY2020 and Excluded in FY2021) |
|||
CMS Star Rating
CMS has implemented a 5-star rating system to evaluate the experiences medicare beneficiaries have with their healthcare service providers. The hospitals are rated on a scale of 1 to 5, with 5 being the highest. While there are no financial incentives linked to the program, the rating determines the reputation of hospitals, and patients are motivated to go with the hospitals that have the highest rating. There is a total of 5 measure groups with each one contributing a different percentage to the overall rating.
| Measure Name | Description | FY 2017 | FY 2019 | FY 2020 | FY 2021 |
| Mortality | |||||
|---|---|---|---|---|---|
| MORT-30-AMI | AMI- 30-day Mortality Rate | ✰ | ✰ | ✰ | ✰ |
| MORT-30-CABG | CABG-30-day Mortality Rate | ✰ | ✰ | ✰ | ✰ |
| MORT-30-COPD | COPD-30-day Mortality Rate | ✰ | ✰ | ✰ | ✰ |
| MORT-30-HF | HF-30-day Mortality Rate | ✰ | ✰ | ✰ | ✰ |
| MORT-30-PN | Pneumonia -30-day Mortality Rate | ✰ | ✰ | ✰ | ✰ |
| MORT-30-STK | Stroke 30-day Mortality Rate | ✰ | ✰ | ✰ | ✰ |
| PSI-4-SURG-COMP | Death rate among surgical inpatients with serious treatable complications | ✰ | ✰ | ✰ | ✰ |
| Safety of Care | |||||
| HAI-1 | CLABSI in ICUs and Select Wards | ✰ | ✰ | ✰ | ✰ |
| HAI-2 | CAUTI in ICUs and Select Wards | ✰ | ✰ | ✰ | ✰ |
| HAI-3 | SSI: Colon | ✰ | ✰ | ✰ | ✰ |
| HAI-4 | SSI: Hysterectomy | ✰ | ✰ | ✰ | ✰ |
| HAI-5 | MRSA - Bloodstream Infections | ✰ | ✰ | ✰ | ✰ |
| HAI-6 | C.diff. - Intestinal Infections | ✰ | ✰ | ✰ | ✰ |
| COMP-HIP-KNEE | Risk-Standardized Complication Rate - Following elective primary THA and TKA | ✰ | ✰ | ✰ | ✰ |
| PSI-90-Safety | Patient safety and adverse events composite | ✰ | ✰ | ✰ | ✰ |
| Readmission | |||||
| READM-30-CABG | CABG - Surgery 30-day Readmission Rate | ✰ | ✰ | ✰ | ✰ |
| READM-30-COPD | COPD- 30-day Readmission Rate | ✰ | ✰ | ✰ | ✰ |
| READM-30-Hip-Knee | 30-day readmission rate following elective primary THA and/or TKA | ✰ | ✰ | ✰ | ✰ |
| READM-30-HOSP-WIDE | 30-day hospital-wide all- cause unplanned readmission (HWR) | ✰ | ✰ | ✰ | ✰ |
| EDAC-30-AMI | AMI - Excess Days in Acute Care | ✰ | ✰ | ✰ | ✰ |
| EDAC-30-HF | HF - Excess Days in Acute Care | ✰ | ✰ | ✰ | ✰ |
| EDAC-30-PN | PN - Excess Days in Acute Care | ✰ | ✰ | ✰ | ✰ |
| OP-32 | Facility 7-day risk standardized hospital visit rate after outpatient colonoscopy | ✰ | ✰ | ✰ | ✰ |
| READM-30-STK | Stroke -30-Day Readmission Rate | ✰ | |||
| Patient Experience | |||||
| H-CLEAN-HSP | Cleanliness of Hospital Environment | ✰ | ✰ | ✰ | ✰ |
| H-COMP-1 | Communication with Nurses | ✰ | ✰ | ✰ | ✰ |
| H-COMP-2 | Communication with Doctors | ✰ | ✰ | ✰ | ✰ |
| H-COMP-3 | Responsiveness of Hospital Staff | ✰ | ✰ | ✰ | ✰ |
| H-COMP-5 | Communication about Medicines | ✰ | ✰ | ✰ | ✰ |
| H-COMP-6 | Discharge Information | ✰ | ✰ | ✰ | ✰ |
| H-HSP-RATING | Overall Rating of Hospital | ✰ | ✰ | ✰ | ✰ |
| H-QUIET-HSP | Quietness of Hospital Environment | ✰ | ✰ | ✰ | ✰ |
| H-RECMND | Willingness to Recommend the Hospital | ✰ | ✰ | ✰ | ✰ |
| H-COMP-7 | Care Transition | ✰ | ✰ | ✰ | ✰ |
| Timely and Effective Care | |||||
| IMM-2 | Influenza immunization | ✰ | ✰ | ✰ | |
| IMM-3 | Influenza vaccination coverage among healthcare personnel | ✰ | ✰ | ✰ | |
| OP-22 | Left without being seen | ✰ | ✰ | ✰ | ✰ |
| OP-23 | Head CT scan results for acute ischemic stroke or hemorrhagic stroke who received head CT scan interpretation within 45 minutes of arrival | ✰ | ✰ | ✰ | ✰ |
| OP-29 | Appropriate follow-up interval for normal colonoscopy in average risk patients | ✰ | ✰ | ✰ | ✰ |
| OP-30 | Colonoscopy interval for patients with a history of adenomatous polyps - avoidance of inappropriate use | ✰ | ✰ | ✰ | |
| OP-33 | External beam radiotherapy for bone metastases | ✰ | ✰ | ✰ | ✰ |
| PC-01 | Elective delivery prior to 39 completed weeks of gestation | ✰ | ✰ | ✰ | ✰ |
| SEP-1 | Early management bundle, severe sepsis/septic shock | ✰ | ✰ | ✰ | ✰ |
| VTE-6 | Hospital acquired potentially preventable venous thromboembolism | ✰ | ✰ | ✰ | |
| OP-4 | Aspirin at Arrival | ✰ | |||
| ED-1b | Average (median) time patients spent in the emergency department, before they were admitted to the hospital as an inpatient A lower number of minutes is better | ✰ | ✰ | ✰ | |
| ED-2b | Median time from admit decision to time of departure from the emergency department for patients admitted to inpatient status | ✰ | ✰ | ✰ | ✰ |
| OP-2 | Fibrinolytic therapy received within 30 minutes of emergency department arrival | ✰ | ✰ | ✰ | ✰ |
| OP-3b | Median time to transfer to another facility for acute coronary intervention | ✰ | ✰ | ✰ | ✰ |
| OP-5 | Median Time to ECG | ✰ | ✰ | ✰ | |
| OP-18b | Median time from emergency department arrival to emergency department departure for discharged patients | ✰ | ✰ | ✰ | ✰ |
| OP-1 | Median Time to Fibrinolysis | ✰ | |||
| OP-20 | Door to Diagnostic Evaluation by a Qualified Medical Professional | ✰ | |||
| OP-21 | Median Time to Pain Management for Long Bone Fracture | ✰ | |||
| OP-8 | MRI lumbar spine for low back pain | ✰ | ✰ | ✰ | ✰ |
| OP-10 | Abdomen CT - use of contrast material | ✰ | ✰ | ✰ | ✰ |
| OP-11 | Thorax CT Use of Contrast Material | ✰ | ✰ | ✰ | |
| OP-13 | Cardiac imaging for preoperative risk assessment for non-cardiac low-risk surgery | ✰ | ✰ | ✰ | ✰ |
| OP-14 | Outpatients with brain CT scans who got a sinus CT scan at the same time | ✰ | ✰ | ✰ | |

Generally, the four outcome measure groups (Mortality, Safety of Care, Patient Experience, Timely and Effective Care) were weighted at 22% each, and the three process measure groups (Effectiveness of Care, Timeliness of care, Efficient Use of Medical Imaging) were weighted at 4% each in FY 2017, 2019, and 2020. In FY 2021, four outcome measure groups' weightage remain the same at 22% and three process measure groups (Effectiveness of Care, Timeliness of Care, and Efficient Use of Medical Imaging) are consolidated into one process measure group called Timely and Effective Care with a weightage of 12%.
Value Based Purchasing
The hospital Value-Based Purchasing (VBP) program was implemented to improve the clinical outcomes, efficiency, safety of patients during the inpatient stays. CMS has developed different metrics to evaluate the performance of the hospitals and provide financial incentives to hospitals based on the measures. CMS has grouped these measures under four domains namely: Clinical outcomes, Efficiency and Cost reduction, Safety, and Person and Community engagement. Each domain weighs 25% of the Total Performance Score.
| Measure | Payment Year VBP Program | ||||||
| FY 2020 | FY 2021 | FY 2022 | FY 2023 | FY 2024 | FY 2025 | FY 2026 | |
| Clinical Outcomes | |||||||
|---|---|---|---|---|---|---|---|
| Baseline Year (AMI mortality, HF mortality, COPD mortality, CABG mortality) Note: COPD mortality is applicable from 2021, CABG mortality is applicable from 2022 |
07/01/2010 - 06/30/2013 | 07/01/2011 - 06/30/2014 | 07/01/2012 - 06/30/2015 | 07/01/2013 - 06/30/2016 | 07/01/2014 - 06/30/2017 | 07/01/2015 - 06/30/2018 | 07/01/2016 - 06/30/2019 |
| Performance Year (AMI mortality, HF mortality, COPD mortality, CABG mortality) Note: COPD mortality is applicable from 2021, CABG mortality is applicable from 2022 |
07/01/2015 - 06/30/2018 | 07/01/2016 - 06/30/2019 | 07/01/2017 - 06/30/2020 | 07/01/2018 - 06/30/2021 | 07/01/2019 - 06/30/2022 | 07/01/2020 - 06/30/2023 | 07/01/2021 - 06/30/2024 |
| PN mortality Baseline Year | 07/01/2010 - 06/30/2013 | 07/01/2012 - 06/30/2015 | 07/01/2012 - 06/30/2015 | 07/01/2013 - 06/30/2016 | 07/01/2014 - 06/30/2017 | 07/01/2015 - 06/30/2018 | 07/01/2016 - 06/30/2019 |
| PN mortality Performance Year | 07/01/2015 - 06/30/2018 | 09/01/2017 - 06/30/2019 | 09/01/2017 - 06/30/2020 | 07/01/2018 - 06/30/2021 | 07/01/2019 - 06/30/2022 | 07/01/2020 - 06/30/2023 | 07/01/2021 - 06/30/2024 |
| THA/TKA complications Baseline Year | 07/01/2010 - 06/30/2013 | 04/01/2011 - 03/31/2014 | 04/01/2012 - 03/31/2015 | 04/01/2013 - 03/31/2016 | 04/01/2014 - 03/31/2017 | 04/01/2015 - 03/31/2018 | 04/01/2016 - 03/31/2019 |
| THA/TKA complications Performance Year | 07/01/2015 - 06/30/2018 | 04/01/2016 - 03/31/2019 | 04/01/2017 - 03/31/2020 | 04/01/2018 - 03/31/2021 | 04/01/2019 - 03/31/2022 | 04/01/2020 - 03/31/2023 | 04/01/2021 - 03/31/2024 |
| AMI mortality | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ |
| HF mortality | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ |
| PN mortality | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ |
| THA/TKA complications | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ |
| COPD mortality | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ | |
| CABG mortality | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ | ||
| HCAHPS/Patient Experience | |||||||
| Baseline Year | 01/01/2016 - 12/31/2016 | 01/01/2017 - 12/31/2017 | 01/01/2018 - 12/31/2018 | 01/01/2019 - 12/31/2019 | 01/01/2020 - 12/31/2020 | 01/01/2021 - 12/31/2021 | 01/01/2022 - 12/31/2022 |
| Performance Year | 01/01/2018 - 12/31/2018 | 01/01/2019 - 12/31/2019 | 01/01/2020 - 12/31/2020 | 01/01/2021 - 12/31/2021 | 01/01/2022 - 12/31/2022 | 01/01/2023 - 12/31/2023 | 01/01/2024 - 12/31/2024 |
| H-CLEAN-HSP | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ |
| H-COMP-1 | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ |
| H-COMP-2 | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ |
| H-COMP-3 | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ |
| H-COMP-5 | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ |
| H-COMP-6 | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ |
| H-HSP-RATING | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ |
| H-QUIET-HSP | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ |
| H-RECMND | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ |
| H-COMP-7 | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ |
| Efficiency and Cost Reduction | |||||||
| Baseline Year | 01/01/2016 - 12/31/2016 | 01/01/2017 - 12/31/2017 | 01/01/2018 - 12/31/2018 | 01/01/2019 - 12/31/2019 | 01/01/2020 - 12/31/2020 | 01/01/2021 - 12/31/2021 | 01/01/2022 - 12/31/2022 |
| Performance Year | 01/01/2018 - 12/31/2018 | 01/01/2019 - 12/31/2019 | 01/01/2020 - 12/31/2020 | 01/01/2021 - 12/31/2021 | 01/01/2022 - 12/31/2022 | 01/01/2023 - 12/31/2023 | 01/01/2024 - 12/31/2024 |
| Medicare Spending Per Beneficiary (MSPB) - Hospital | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ |
| Safety | |||||||
| CMS PSI-90 Patient Safetyand Adverse Events Composite Baseline Year | 10/01/2015 - 06/30/2017 | 07/01/2016 - 06/30/2018 | 07/01/2017 - 06/30/2019 | 07/01/2018 - 06/30/2020 | |||
| CMS PSI-90 Patient Safetyand Adverse Events Composite Performance Year | 07/01/2019 - 06/30/2021 | 07/01/2020 - 06/30/2022 | 07/01/2021 - 06/30/2023 | 07/01/2022 - 06/30/2024 | |||
| Baseline Year (CLABSI, CAUTI, SSI, MRSA, C diff, PC-01 Elective delivery) | 01/01/2016 - 12/31/2016 | 01/01/2017 - 12/31/2017 | 01/01/2018 - 12/31/2018 | 01/01/2019 - 12/31/2019 | 01/01/2020 - 12/31/2020 | 01/01/2021 - 12/31/2021 | 01/01/2022 - 12/31/2022 |
| Performance Year (CLABSI, CAUTI, SSI, MRSA, C diff, PC-01 Elective delivery) | 01/01/2018 - 12/31/2018 | 01/01/2019 - 12/31/2019 | 01/01/2020 - 12/31/2020 | 01/01/2021 - 12/31/2021 | 01/01/2022 - 12/31/2022 | 01/01/2023 - 12/31/2023 | 01/01/2024 - 12/31/2024 |
| CMS PSI-90 Patient Safetyand Adverse Events Composite | ⊜ | ⊜ | ⊜ | ⊜ | |||
| CLABSI | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ |
| CAUTI | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ |
| SSI | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ |
| MRSA | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ |
| C diff | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ | ⊜ |
| PC-01 Elective delivery | ⊜ | ||||||
Hospitals Readmissions Reduction Program
HRRP is intended to improve the communication and coordination between caregivers and patients in developing discharge plans to avoid possible readmissions. The program achieves the goal by linking payments to value outcomes. CMS considers 6 conditions as part of the program and calculates the 30-day readmission measure. The payments are determined based on the performance of the hospital during a 3-year period.
Acute myocardial infarction (AMI)
Chronic obstructive pulmonary disease (COPD)
Heart failure (HF)
Pneumonia
Coronary artery bypass graft (CABG) surgery
Elective primary total hip arthroplasty and/or total knee arthroplasty (THA/TKA)
*Abbreviated performance periods due to the data exclusions stipulated in an Interim Final Rule (CMS-3401-IFC) which specifies that CMS will exclude claims data and HAI data that hospitals have submitted for Q1 2020 and Q2 2020 from program calculations for the HRRP.
| Measure | Payment Year in HRRP | ||||
| FY 2020 | FY 2021 | FY 2022 | FY 2023 | ||
| Performance Periods | 07/01/2015 - 06/30/2018 | 07/01/2016 - 06/30/2019 | 07/01/2017 - 12/31/2019* | 07/01/2018 - 12/31/2019 & 07/01/2020 - 06/30/2021* |
|
| AMI readmissions | ⇄ | ⇄ | ⇄ | ⇄ | |
| HF readmissions | ⇄ | ⇄ | ⇄ | ⇄ | |
| PN readmissions | ⇄ | ⇄ | ⇄ | ⇄ | |
| THA/TKA readmissions | ⇄ | ⇄ | ⇄ | ⇄ | |
| COPD readmissions | ⇄ | ⇄ | ⇄ | ⇄ | |
| CABG readmissions | ⇄ | ⇄ | ⇄ | ⇄ | |

Hospital-Acquired Condition Reduction Program
Through this program, CMS aims to reduce hospital-acquired infections that occur as a result of negligence and improve the quality of care during inpatient stays. CMS links financial payments to the HAC measures to encourage hospitals to improve their score. CMS uses the total HAC score to determine the lowest-scoring hospitals and reduces payment while paying the medicare claims. The total HAC score is calculated using 6 measures:
Patient Safety Indicator (PSI) 90
Central Line-Associated Bloodstream Infection (CLABSI)
Catheter-Associated Urinary Tract Infection (CAUTI)
Surgical Site Infection (SSI) – colon and hysterectomy
Methicillin-resistant Staphylococcus aureus (MRSA) bacteremia
Clostridium difficile Infection (CDI)
*Abbreviated performance periods due to the data exclusions stipulated in an Interim Final Rule (CMS-3401-IFC) which specifies that CMS will exclude claims data and HAI data that hospitals have submitted for Q1 2020 and Q2 2020 from program calculations for the HAC Reduction Program.
| Measure | Payment Year HAC Program | ||||
| FY 2020 | FY 2021 | FY 2022 | FY 2023 | ||
| CMS PSI-90 Patient safety for selected indicators (composite) Performance Periods | 07/01/2016 - 06/30/2018 | 07/01/2017 - 06/30/2019 | 07/01/2018 - 12/31/2019* | 07/01/2019 - 12/31/2019 & 07/01/2020 - 06/30/2021* |
|
| Performance Periods (CLABSI, CAUTI, Colon and Abdominal Hysterectomy SSI, MRSA Bacteremia, CDI Clostridium difficile Infection) | 01/01/2017 - 12/31/2018 | 01/01/2018 - 12/31/2019 | 01/01/2019 - 12/31/2019 & 07/01/2020 - 12/31/2020* |
07/01/2020 - 12/31/2021* | |
| CMS PSI-90 Patient safety for selected indicators (composite) | ⊕ | ⊕ | ⊕ | ⊕ | |
| CLABSI | ⊕ | ⊕ | ⊕ | ⊕ | |
| CAUTI | ⊕ | ⊕ | ⊕ | ⊕ | |
| Colon and Abdominal Hysterectomy SSI | ⊕ | ⊕ | ⊕ | ⊕ | |
| MRSA Bacteremia | ⊕ | ⊕ | ⊕ | ⊕ | |
| CDI Clostridium difficile Infection | ⊕ | ⊕ | ⊕ | ⊕ | |

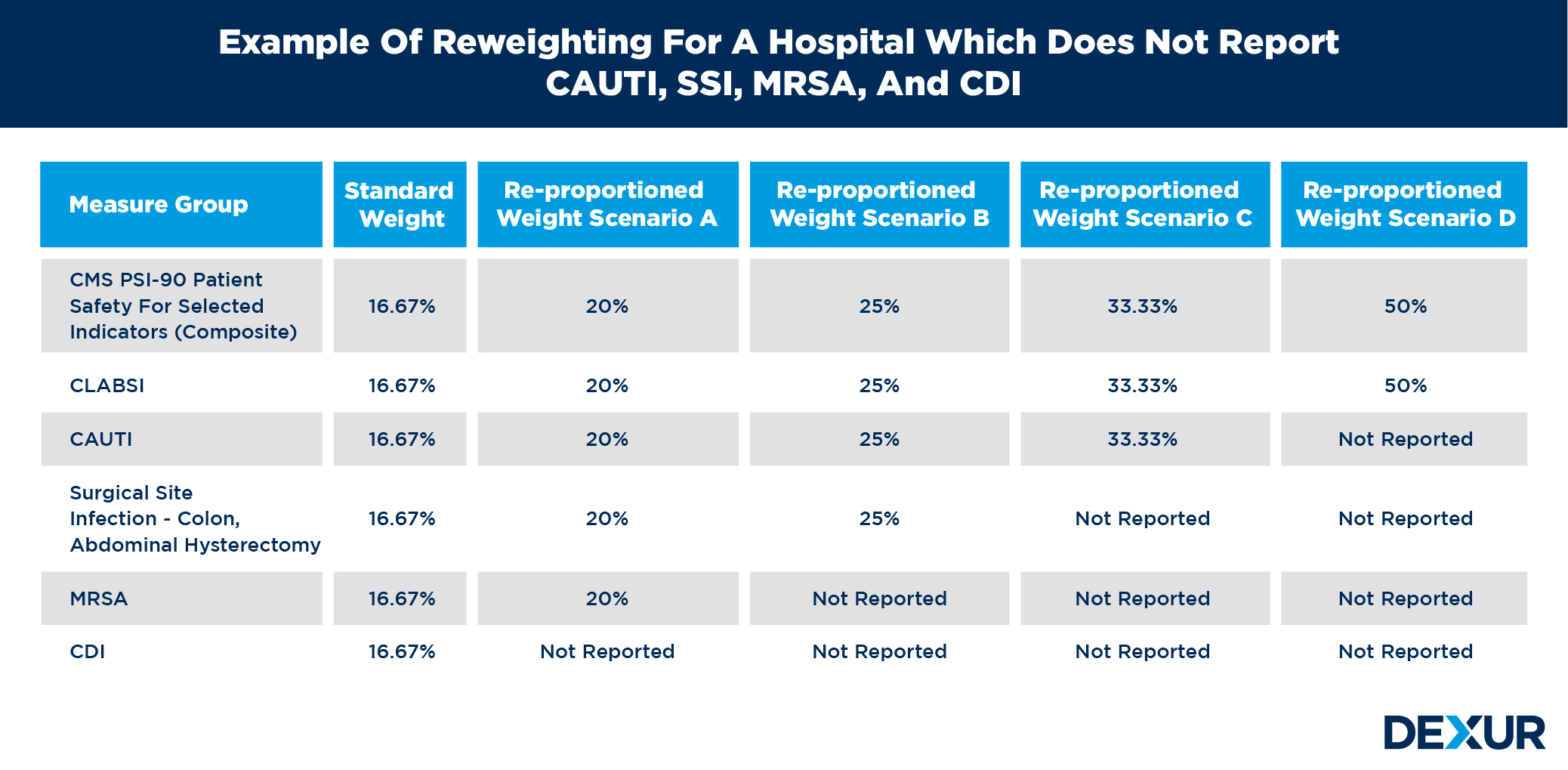
CMS finalized the adoption of the Equal Measure Weights approach in the FY 2019. The Equal Measure Weights approach applies an equal weight to each measure for which a hospital has a measure score. In the following diagram standard weight for each measure is 16.67% when hospital has all 6 measures score. In Re-proportioned Weight Scenario A, hospital has 5 measures score and weight for each measure is 20% as per Equal Measure Weights approach. In Re-proportioned Weight Scenario B, hospital has 4 measures score and weight for each measure is 25% as per Equal Measure Weights approach. In Re-proportioned Weight Scenario C, hospital has 3 measures score and weight for each measure is 33.33% as per Equal Measure Weights approach. In Re-proportioned Weight Scenario D, hospital has 2 measures score and weight for each measure is 50% as per Equal Measure Weights approach.
CMS takes an extended amount of time in calculating the measures and releasing the scores to healthcare service providers. Hospitals can not devise any actionable plans to address the low scoring areas due to the time delay. Dexur replicates the same algorithms and provides data at DRG levels at a much faster rate to help hospitals develop specific plans to improve their score.
Impact of different measures on CMS programs
Mortality Rates
The mortality rate is an important metric that has a significant weightage in different CMS programs. It weighs 22% in the CMS Star Rating program and 25% in the VBP program under the Clinical Outcomes domain. Dexur provides the mortality rates for different time periods at DRG levels to help hospitals understand their performance. Hospitals can give special attention to conditions that have a high mortality rate and come up with specific treatment plans to improve their score. Only certain conditions are taken into account in calculating the mortality score for VBP and Star Rating program.
AMI 30 Day Mortality Rate
CABG 30 Day Mortality Rate
COPD 30 Day Mortality Rate
Heart Failure 30 Day Mortality Rate
Pneumonia 30 Day Mortality Rate
Stroke 30-day Mortality Rate
Death rate among surgical inpatients with serious treatable complications
Safety/Hospital-Acquired Conditions
Safety is another important metric that impacts multiple CMS programs. The safety measure forms an integral part of VBP program contributing 25% to it. The metric also weighs 22% in the star rating program. The metric is used to assess the safety aspect of hospitals and prevent the occurrence of infections during the inpatient stay.
MSPB
MSPB is the sole metric used to calculate the Efficiency and Cost reduction domain in the VBP program. It measures the cost to Medicare for services performed by healthcare providers. The costs incurred from 3-day prior admission period to 30-day post-discharge is used to calculate the MSPB costs. In order to calculate the MSPB for each hospital, Dexur determined the time frame of the spending per beneficiary episode during which Medicare payments would be aggregated and the type of Medicare payments to be aggregated over this time frame. See Dexur’s MSPB features here.
Readmission Rates
The readmission rate weighs 22% in the star rating program and also has a significant impact on the VBP program under the MSPB domain. The star rating program only considers the readmission rate of certain conditions, the same ones used to calculate the mortality rate. The readmission rates are calculated post 30 days from the discharge period.
HCAHPS scores
CMS uses the HCAHPS score to calculate the Personal and Community Engagement domain in the VBP program and Patient Experience in the star rating program. CMS developed a standardized survey of patient’s healthcare experience in collaboration with AHRQ (Agency for Healthcare Research and Quality). The survey is comprised of 27 questions that measure a patient’s experience with:
Communication with healthcare service providers
Information about medicines
3-item care transition
Responsiveness
Hospital hygiene
Discharge information
Overall rating of the hospital
The survey is not limited to Medicare beneficiaries and any patient who has spent at least one night in a hospital facility can participate in the survey. The patients would be requested to fill the survey from 48 hours to 6 weeks after the discharge.
Timely and Effective Care Measures
The measures of timely and effective care, also known as process of care measures, part of the CMS Star-Rating, show how often or how quickly hospitals provide care that research shows gets the best results for patients with cataract surgery, a colonoscopy, a heart attack, emergency department care, preventative care, a stroke, a blood clot, or childbirth. Hospitals voluntarily submit data from their medical records about the treatments their patients receive for these conditions, including patients with Medicare and those who do not have Medicare.
Efficient Use of Medical Imaging
The measures on the use of medical imaging show how often a hospital provides specific imaging tests for Medicare beneficiaries under circumstances where the imaging may not be medically appropriate. Lower percentages suggest more efficient use of medical imaging. The measure is only aplicaple for Medicare patients who were treated in an outpatient setting. Measures included in calculator of CMS Star Rating are as following:
MRI lumbar spine for low back pain
Abdomen CT - use of contrast material
Thorax CT Use of Contrast Material
Cardiac imaging for preoperative risk assessment for non-cardiac low-risk surgery
Outpatients with brain CT scans who got a sinus CT scan at the same time