Precision Medicine May Help Catch Idiopathic Pulmonary Fibrosis at Large Hospitals
In Interstitial Lung Disease (ILD)
Get Dexur’s Personalized Hospital Specific Presentation on Quality, Safety, Compliance & Education
By: James Pitt May. 18, 2018
Interstitial lung disease (ILD) includes over 100 disorders with varying treatments and prognoses. Idiopathic pulmonary fibrosis (IPF) is according to the Cleveland Clinic the second most common ILD. IPF has a poor prognosis: “The majority of patients die of progressive fibrosing lung disease within 4 years of diagnosis.”
In the past few years several treatment approaches were found to do more harm than good. However, two new IPF treatments earned FDA approval in 2014. In randomized controlled trials of nintedanib and pirfenidone, forced vital capacity (a measure of lung function) decreased about half as much in the treatment group as the control group.
These new treatments make an IPF diagnosis more actionable than in the past. But diagnosis remains difficult. CT scans are often inconclusive, prompting preliminary research on machine vision to detect IPF from CT scans. A promising approach is “precision medicine,” the use of statistics and machine learning to identify specific subtypes of disease that are more susceptible to specific treatments. Several biomarkers are known for IPF, and a 2017 paper found that machine learning could categorize IPF using RNA from a transbronchial biopsy. This is less invasive than the lung biopsy that would otherwise be required.
To estimate the scope of need for new medications and diagnostic tests for IPF in ILD patients, Dexur analysts examined ILD discharges among CMS inpatients at large US hospitals from 2013-2016.
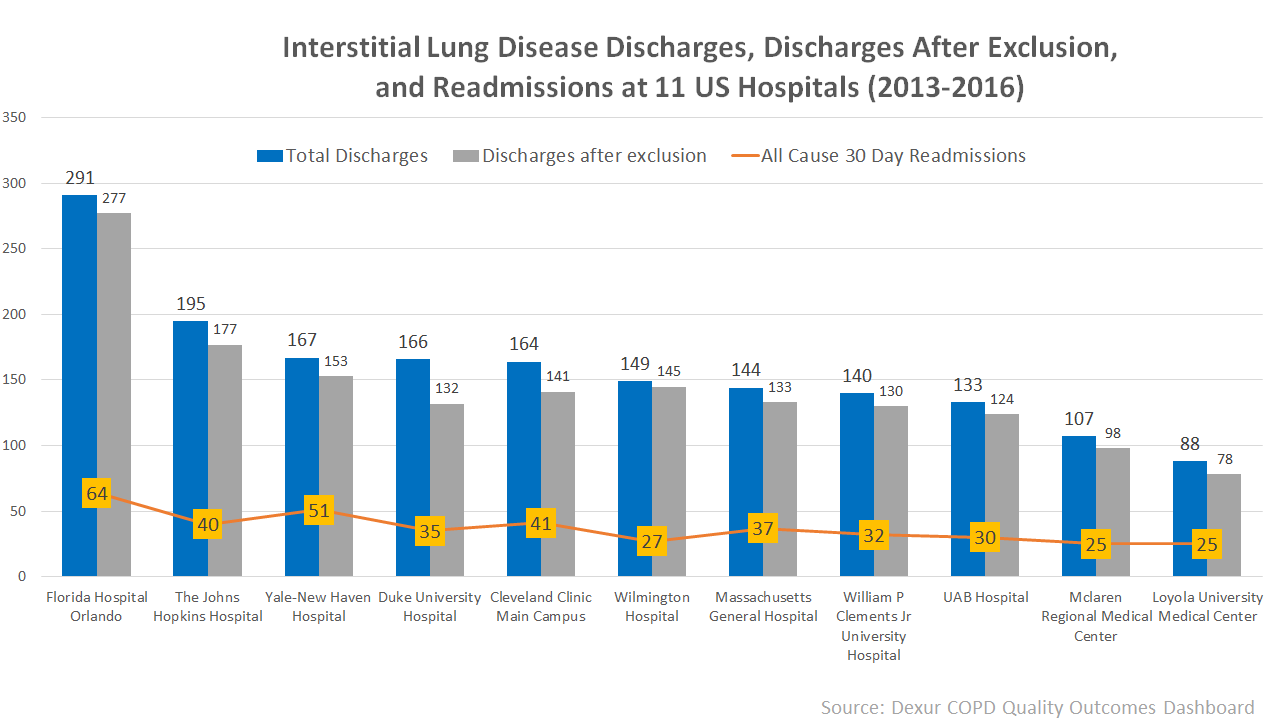
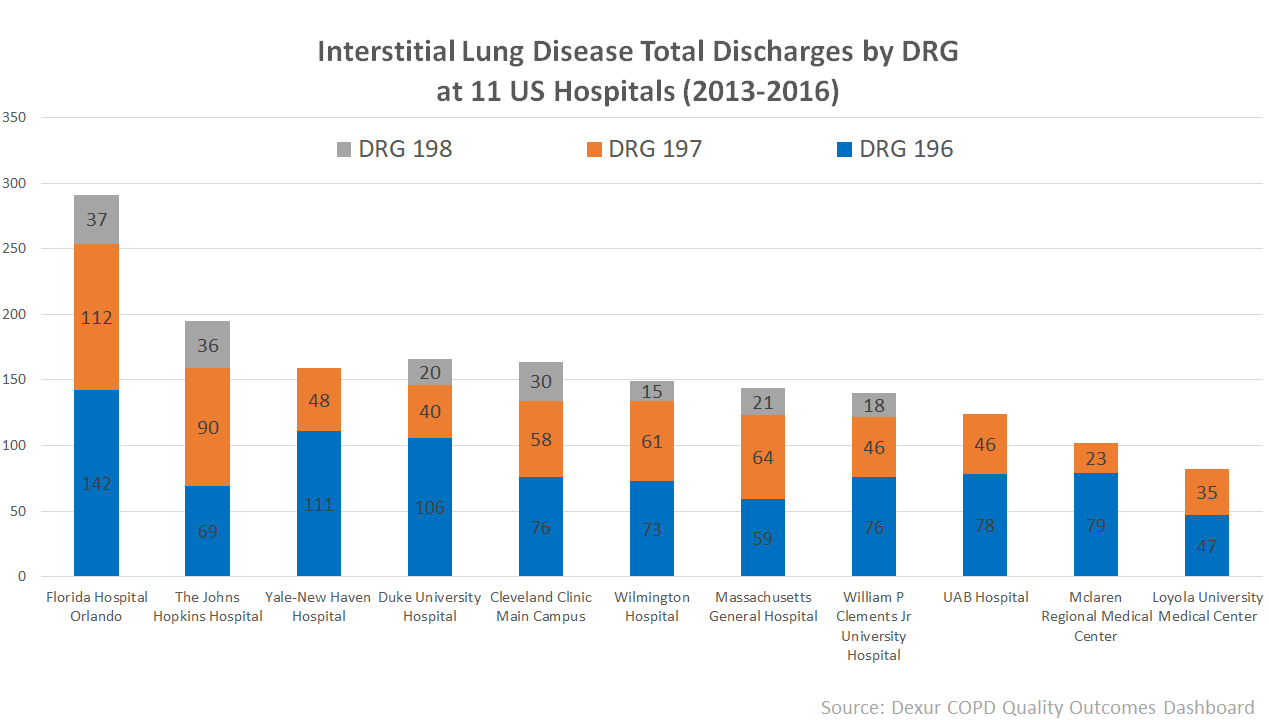
30-day all-cause readmission rates for ILD patients were generally over 20%. The highest was 33% at Yale - New Haven Hospital (New Haven, CT), and the lowest 19% at Wilmington Hospital (Wilmington, DE). Higher readmission rates tended to be at hospitals with greater proportions of patients with major complications (DRG 196) or complications (DRG 197), reflecting a patient population with greater risks. (Hospitals for which DRG 198 is not shown reported fewer than 10 DRG 198 patients).
A May 2018 review in New England Journal of Medicine found increasing hospital admission and death rates for IPF. As the burden of IPF grows, improved treatment and diagnosis will become increasingly important.
DEXUR PRO MEMBERS GET ACCESS TO:
- Total discharges for all interstitial lung disease
- DRG 196 discharges
- DRG 197 discharges
- DRG 198 discharges
- Discharges excluding patients who expired, were transferred, or were discharged against medical advice for all interstitial lung disease
- DRG 196 discharges after exclusion
- DRG 197 discharges after exclusion
- DRG 198 discharges after exclusion
- All cause 30 day readmissions for all interstitial lung disease
- All cause 30 day readmissions rate for all interstitial lung disease
From 2013-2016, for patients at Cleveland Clinic Main Campus (Cleveland, OH), Duke University Hospital (Durham, North Carolina), Florida Hospital Orlando (Orlando, Florida), Loyola University Medical Center (Maywood, Illinois), Massachusetts General Hospital (Massachusetts, Boston), Mclaren Regional Medical Center (Flint, Michigan), The Johns Hopkins Hospital (Baltimore, Maryland), UAB Hospital (Birmingham, Alabama), William P Clements Jr University Hospital (Dallas, Texas), Wilmington Hospital (Wilmington, Delaware), and Yale-New Haven Hospital (New Haven, Connecticut)
ABOUT THE AUTHOR
