Get Dexur’s Personalized Hospital Specific Presentation on Quality, Safety, Compliance & Education
These articles are from Dexur's Rural Health Newsletter, which is focused on Rural Healthcare’s operations, technology, quality, safety, risk, compliance and learning topics. Please email DexurRuralHealth@dexur4.com to join this newsletter and receive updates (not more than once per week).
Dexur Rural Health Insights
Imagine you're in a routine leadership meeting, presenting your hospital's latest quality metrics from your internal dashboard—readmission rates, and mortality metrics, all seemingly well under control. The team is satisfied and confident in the data's accuracy and the hospital’s performance. Fast forward to the release of the Centers for Medicare & Medicaid Services (CMS) final results, and the situation unfolds quite differently. Suddenly, there’s a stark contrast—CMS data indicates a decline in performance. The board is stunned, the C-suite is questioning the data, and you're left wondering where the discrepancy lies.
Read moreMedical coding and quality improvement teams can effectively leverage data on risk factors that influence specific readmission and mortality measures to enhance healthcare outcomes. By ensuring accurate medical coding, these teams can identify discrepancies and opportunities for improvement, leading to more precise documentation and better resource allocation. Quality improvement teams can utilize this data to target interventions for high-risk patient cohorts, thereby reducing readmission rates and improving care quality. Collaboration between coding and quality teams, informed by comprehensive risk factor analysis, is crucial in driving operational efficiencies and enhancing patient care. This synergy not only supports financial performance through improved coding and reimbursement accuracy but also fosters a culture of continuous quality improvement within healthcare organizations.
Read more48% of SSI Colon Hospital Acquired infections are likely to occur within 10 days of Admission
Importance and Background on Surgical Site Infections in the Colon
Surgical Site Infections (SSI) following colon surgery present a significant challenge in healthcare. They adversely affect patient recovery and impact hospital quality metrics. These infections not only lead to longer hospital stays and increased costs but can also result in severe, life-threatening complications. Therefore, it is essential to focus on enhancing infection control measures and implementing robust post-surgical care protocols to effectively prevent and manage these infections.
Read moreThis white paper highlights how healthcare organizations can significantly reduce costs and enhance operational efficiency by consolidating multiple functions into a single platform with Dexur's AI Unified Quality and Risk Management software. Dexur offers an AI-powered unified system for managing quality, safety, risk, and incidents. By adopting Dexur's integrated software, healthcare providers can streamline their operations and achieve a higher standard of care at a reduced expense.
Read moreKey Pathogens Influencing CAUTI Infections in Hospitals
Catheter-associated Urinary Tract Infections (CAUTI) greatly influence both patient outcomes and the financial aspects of healthcare, with Dexur being a key contributor in data analytics to improve healthcare safety and quality. Leveraging hospital data reported to the CDC's NHSN, Dexur identifies key pathogens contributing to CAUTI, highlighting the top five: Escherichia coli, Pseudomonas aeruginosa, Klebsiella pneumoniae, Enterococcus faecalis, and Proteus mirabilis. Each of these pathogens poses distinct challenges in their treatment and prevention. Through Dexur's detailed analysis, the development of targeted infection control protocols is facilitated, and the process supports both Root Cause Analysis (RCA) and the implementation of Corrective and Preventive Actions (CAPA). Such a strategy is crucial for the effective management of CAUTI, with the ultimate goal of enhancing patient outcomes and the efficiency of healthcare services.
Read moreThe Texas Hospital Association (THA) has endorsed Dexur, an AI-driven unified Quality, Safety, Risk, and Incident Management software, to support its member hospitals. This partnership is highlighted by THA's Alex Huff and Dexur's CEO, Nik Rao, who emphasize the alignment of Dexur's advanced technological capabilities, including AI-driven analytics and comprehensive data management, with THA's goals for enhancing healthcare quality and efficiency. Dexur's platform will offer THA hospitals a suite of tools for detailed program-to-case analysis, predictive insights, and strategic planning aimed at improving patient care outcomes and operational performance at a dramatically cost-effective price.
Read moreA Significant Portion of Readmitted Patients Stay for only 1 or 2 Days
Readmissions are a critical quality metric for hospitals, significantly impacting financial and reputational outcomes under the Hospital Readmissions Reduction Program (HRRP) and the Centers for Medicare & Medicaid Services (CMS) Star Rating system. The HRRP imposes penalties on hospitals with higher-than-expected readmission rates for specific conditions, aiming to incentivize improvements in hospital discharge planning and post-discharge care. Similarly, the CMS Star Rating system evaluates hospitals on various performance measures, including readmission rates, to help consumers compare hospitals more easily. High readmission rates can lead to reduced Medicare payments and lower star ratings, which may influence patient choice and hospital revenue.
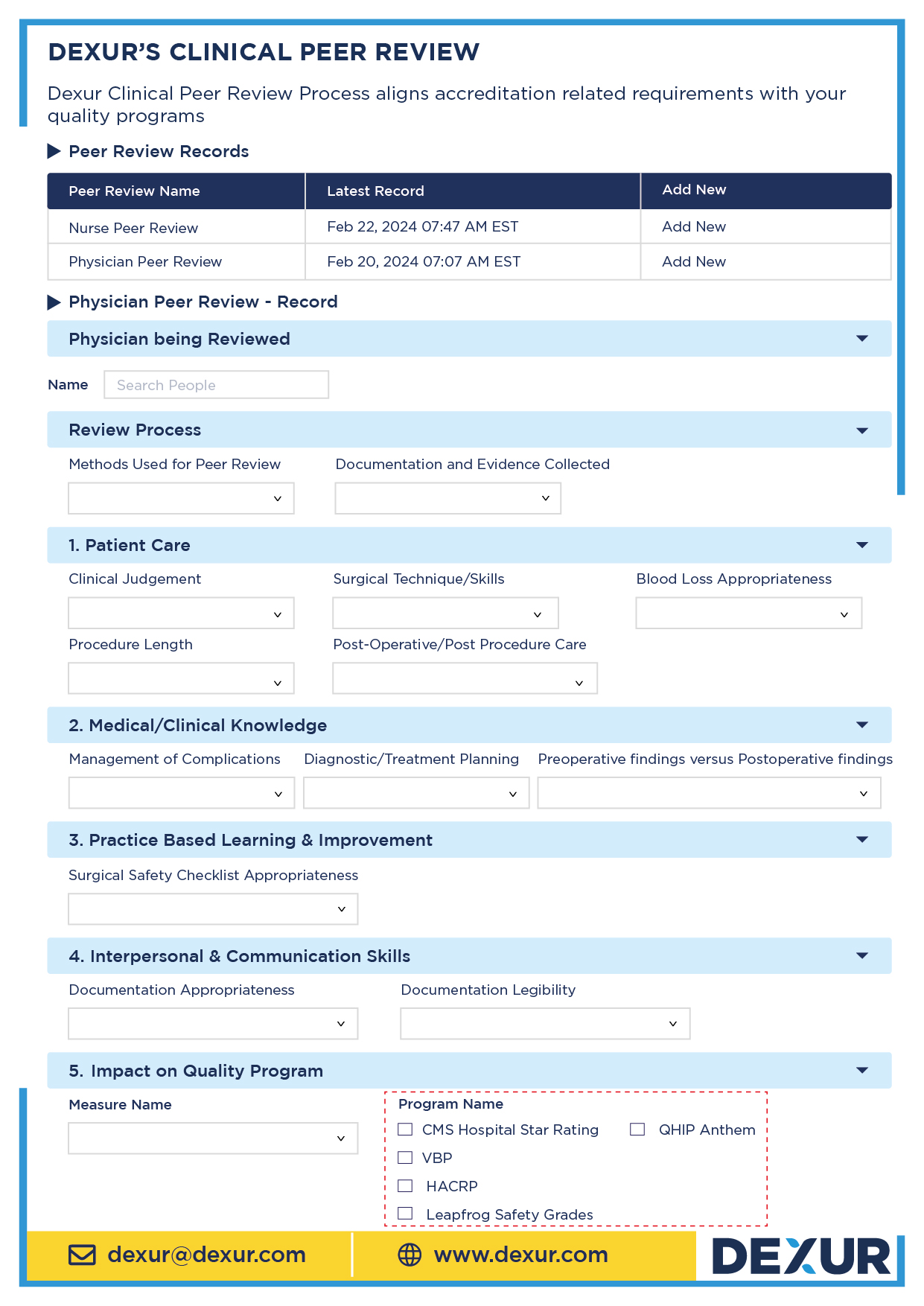
Read morePeer review is a critical component in the accreditation and quality assurance processes for healthcare organizations. The Joint Commission (TJC), the Centers for Medicare & Medicaid Services (CMS), Det Norske Veritas (DNV), and the National Committee for Quality Assurance (NCQA) each have specific expectations regarding peer review processes.
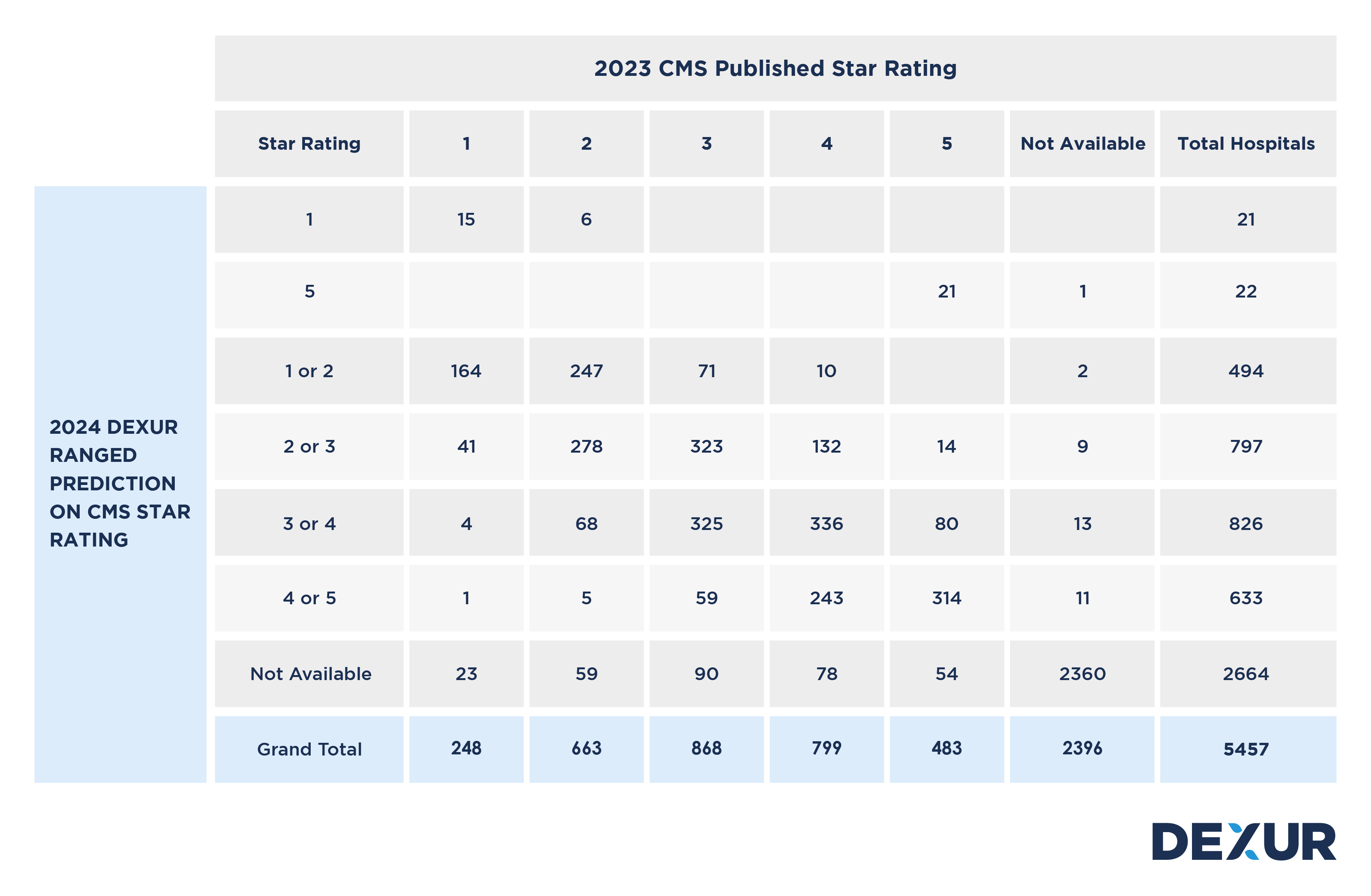
Read moreWebinar: Dexur Releases its Annual 2024 CMS Star Rating Predictions
Dexur makes its annual predictions on CMS Star Ratings before CMS Star Ratings are published in July of every year. In 2023, Dexur had a 98% accuracy rate in its annual prediction rate. To get an understanding of your Hospital’s increase in decrease of your Star Rating, you can search for your Hospital’s prediction via the Hospital Search Function or you can also go through any Hospital’s CMS Star Rating predictions direction by browsing through state pages. To get the actual Star Rating prediction and a glimpse of the key drivers of the performance, you can also reach out to Dexur by email dexur@dexur.com.
Read moreEmergency Departments Play a Critical Role In Managing Readmissions
Readmissions to hospitals, particularly within 30 days of discharge, serve as a critical measure for evaluating the quality and effectiveness of healthcare services. The Hospital Readmission Reduction Program (HRRP) and the Centers for Medicare & Medicaid Services (CMS) Star Rating system place significant emphasis on readmission rates as indicators of hospital performance. These measures directly impact hospitals' financial health through penalties and influence their reputation through public reporting.
Read moreWhy are Inpatient THA / TKA Readmissions and Complications Increasing?
Total Hip Arthroplasty (THA) and Total Knee Arthroplasty (TKA) are critical measures in assessing the quality of care provided by healthcare facilities, particularly in the context of Medicare's value-based care models. These procedures are common among the elderly population, who are the primary beneficiaries of Medicare. The rates of 30-day readmission and complications after THA/TKA are significant indicators of the quality and effectiveness of perioperative care, postoperative management, and the overall health system's ability to provide coordinated care. These metrics directly impact various Centers for Medicare & Medicaid Services (CMS) Quality Programs, such as CMS Star Rating and the Hospital Readmissions Reduction Program (HRRP), which penalizes hospitals with higher than expected readmission rates for certain conditions and procedures, including THA/TKA.
Read moreHow the SEP1 Chart Abstraction Measure can be Integrated into CMS Star Ratings and VBP
The SEP1 chart abstraction measure, a critical component in healthcare quality assessment, plays a pivotal role in evaluating the efficiency and effectiveness of sepsis management in healthcare facilities. Sepsis, a life-threatening response to infection leading to tissue damage, organ failure, and potentially death, requires timely and precise treatment. The SEP1 measure is designed to quantify the quality of this treatment by tracking various parameters, such as the timeliness of antibiotic administration and the completeness of sepsis care.
Read moreWhat are the Top Pathogens Impacting CLABSI Infections in Hospitals
Central Line-Associated Bloodstream Infections (CLABSI) remain a significant challenge in healthcare settings, directly influencing patient outcomes and healthcare costs. CLABSI, a severe infection occurring in patients with central venous catheters, poses risks that extend beyond immediate health concerns, impacting hospital ratings and reimbursement rates.
Read moreDexur, a leading provider of AI-driven unified quality and safety, risk, and incident management software, will acquire the Comparative Outcome Profile (COP) chart abstraction software from the Indiana Hospital Association (IHA). This strategic move aims to bolster Dexur's capabilities in offering comprehensive, AI-powered solutions to healthcare organizations.
Read moreMedical coding plays a crucial role in determining risk-adjusted rates, directly influencing a hospital's performance in quality programs like CMS Star Ratings, HRRP, and VBP. Risk adjustment is essential for equitable evaluations, especially in treating complex patient cases. Detailed coding impacts these risk-adjusted metrics, as seen in a case study of Acme Hospital, where coding accuracy significantly affects quality measures and assessments. A comparative analysis of Acme and Vibrant Hospitals further highlights the importance of precise coding practices in reflecting patient care complexity and ensuring fair evaluations in healthcare quality programs.
Read moreCritical Access Hospitals (CAHs) are essential to the healthcare infrastructure, particularly in rural and remote areas. They often serve as the primary, and sometimes only, source of healthcare for their communities. One of the key performance indicators for these hospitals is the management of Chronic Obstructive Pulmonary Disease (COPD) mortality. This measure not only reflects the quality of care provided but also significantly influences the CMS Star Rating's mortality domain.
Read moreHow Rural Hospitals Can Leverage Telehealth to Improve Mortality Measures Impacting CMS Star Ratings
For rural hospitals mortality measure group weightings could range from 22%-39% and therefore have a significance on CMS Star Ratings. Specifically, measures related to heart failure, Acute Myocardial Infarction (AMI), Coronary Artery Bypass Grafting (CABG), Chronic Obstructive Pulmonary Disease (COPD), and Pneumonia are integral to the mortality measure group in CMS Star Ratings. Addressing these specific conditions effectively can lead to improved outcomes, directly impacting a hospital's CMS Star Rating. Telehealth strategies emerge as innovative solutions to confront these challenges, offering rural hospitals a pathway to enhance patient outcomes in these critical areas and, subsequently, improve their CMS Star Ratings.
Read moreAll MBQIP Measures in One Place
The Medicare Beneficiary Quality Improvement Project (MBQIP) is a voluntary quality improvement initiative aimed at promoting better healthcare outcomes for patients treated in critical access hospitals (CAHs), which are often located in rural areas. MBQIP provides an opportunity for small hospitals to report on quality and outcomes data, fostering a culture of quality improvement and enhancing rural healthcare delivery.
Read moreThe capacity for individualized patient care is a significant metric for healthcare quality and outcomes. In smaller rural hospitals, the scale of operations lends itself to a more personalized approach, particularly when managing chronic conditions such as heart failure (HF), acute myocardial infarction (AMI), pneumonia (PN), and chronic obstructive pulmonary disease (COPD). For these conditions, a typical rural hospital may see fewer than 200 patients over three years as per Centers for Medicare & Medicaid Services (CMS) measures, averaging about five patients monthly. This volume is distinctly manageable compared to larger systems, which often struggle to provide individualized follow-up care due to higher patient numbers.
Read moreSmall Size as an Advantage for Rural Hospitals: Smart Use of Technology + Manual Approaches
In the healthcare industry, large organizations face significant challenges due to their size and complexity. Cross-departmental coordination is a critical requirement to mitigate risk, often leading to bureaucratic inertia. Large hospitals rely on massive, centralized systems designed for economies of scale, but these can be slow and costly to alter. When faced with problems, these institutions typically turn to technology as a solution, inflating capital expenditure (Capex) budgets and return on investment (ROI) benchmarks, thus creating barriers to change.
Read moreRural hospitals, with their smaller size, often face the challenge of limited budgets and resources compared to larger healthcare institutions. Large organizations typically have the luxury to allocate distinct technology and application budgets across various functional departments like Quality, Compliance, Risk, and Learning. Each department independently evaluates and selects applications tailored to its unique needs, an approach that often leads to additional spending on system integration to ensure cross-departmental compatibility.
Read moreRural Health and The Challenges of Low Case Volume: MRSA Case Study
Rural hospitals are essential cornerstones of the communities they serve, yet they face unique challenges in assessing the quality of healthcare services they offer. One significant challenge arises from low patient volumes which, while potentially indicative of effective healthcare or healthier populations, can distort quality metrics. This distortion makes benchmarking performance against national standards a complex endeavor. Through the lens of MRSA (Methicillin-resistant Staphylococcus aureus) infections, we can gain valuable insight into this issue.
Read more