Dexur Simulators and Calculators to manage CMS Quality Programs
To help healthcare providers in managing costs and monitoring CMS quality programs, Dexur has developed several simulators and calculators that provide insights and suggest useful scenarios to administer costs and quality outcomes. Dexur provides Simulators & Calculators for the following quality programs:
- Value Based Purchasing (VBP)
- Medicare Spending Per Beneficiary (MSPB)
- Hospital Readmissions Reduction Programme (HRRP)
- Hospital Acquired Conditions (HAC)
- CMS Star Rating
Dexur Simulators and Calculators to improve VBP Score
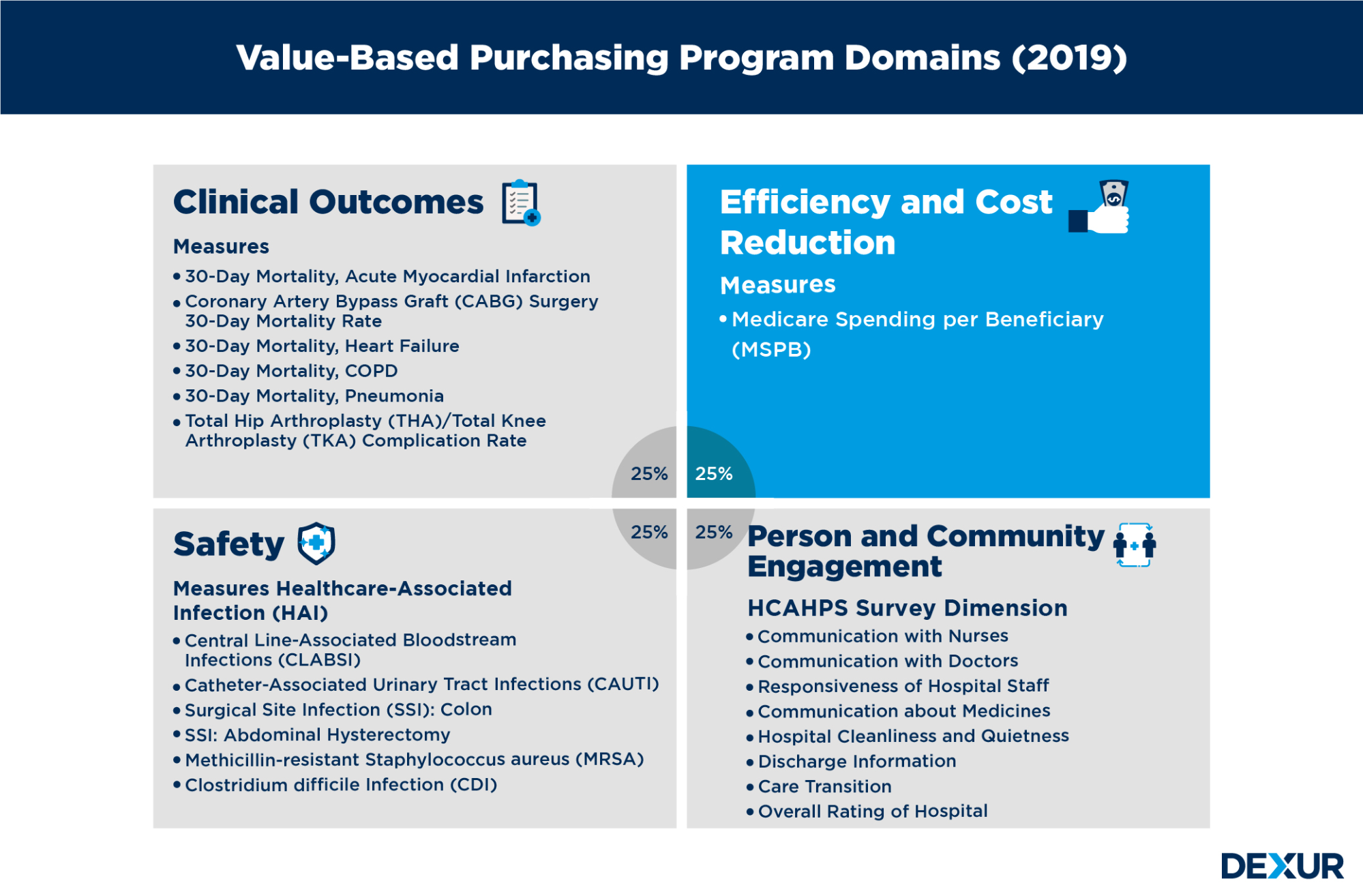
VBP is a CMS program aimed at reducing costs and improving patient experience and safety during inpatient stays.CMS evaluates hospital performance on an approved set of measures and dimensions grouped into four specific quality domains: clinical outcomes, efficiency and cost reduction, safety, and person and community engagement. Domains are assigned equal weights (percentages) of the Total Performance Score.
Dexur Automated Simulator
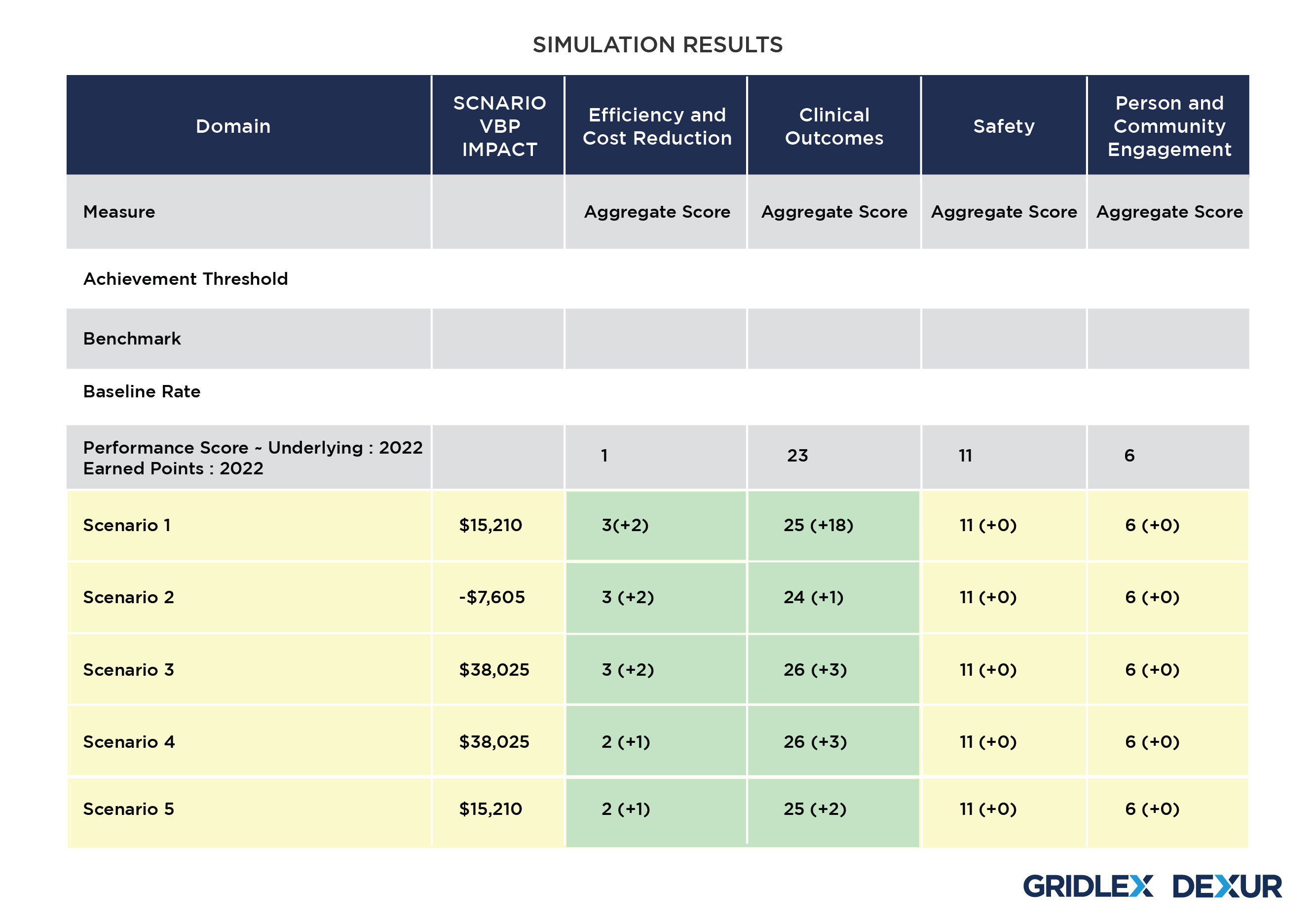
Dexur’s VBP simulator uses scores of all measures in each of these domains and runs permutations to calculate the required improvement in each measure score for achieving the desired VBP impact. The simulator suggests various scenarios with changes in multiple domains for improving VBP and achieving desired financial impact.
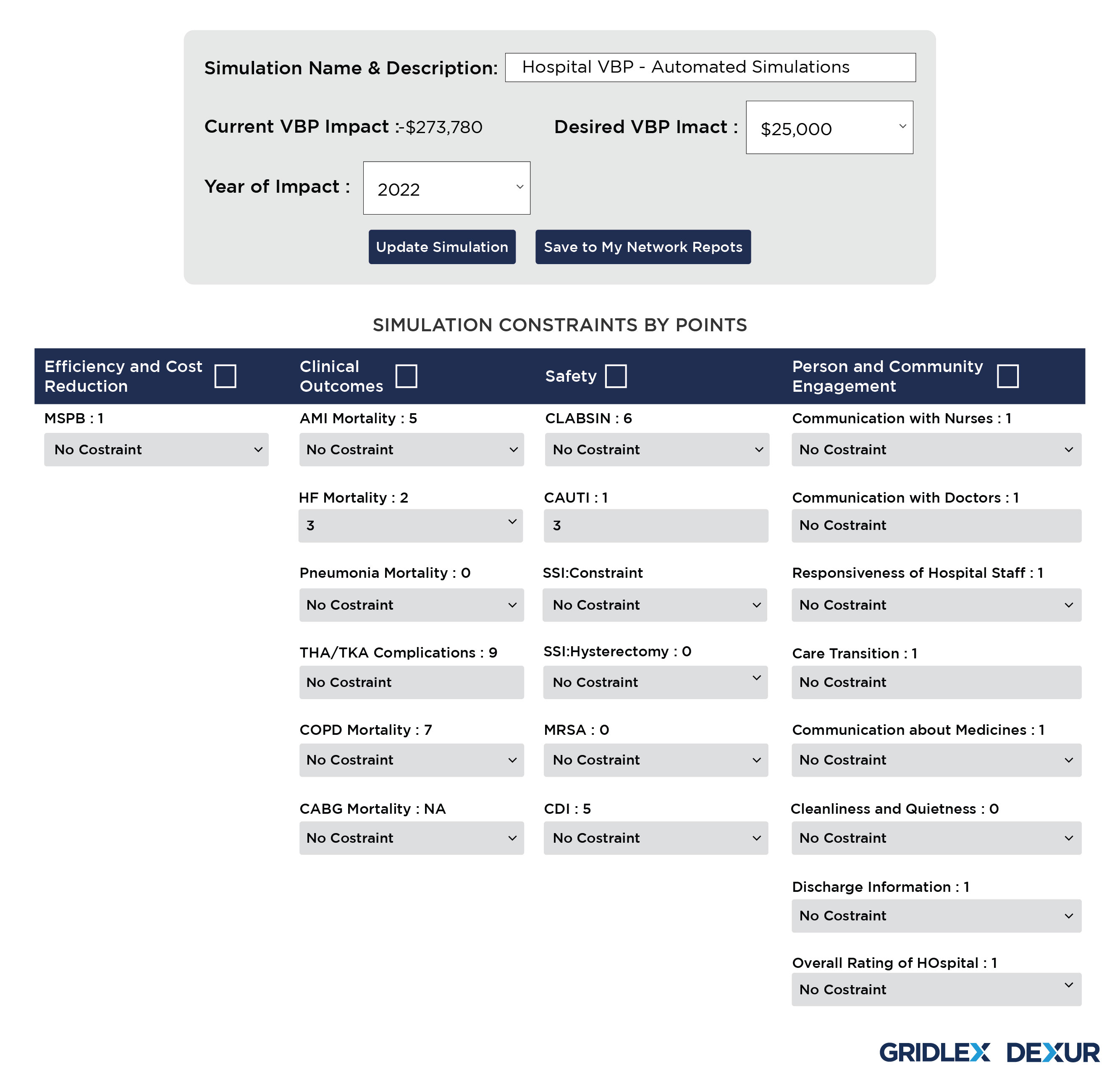
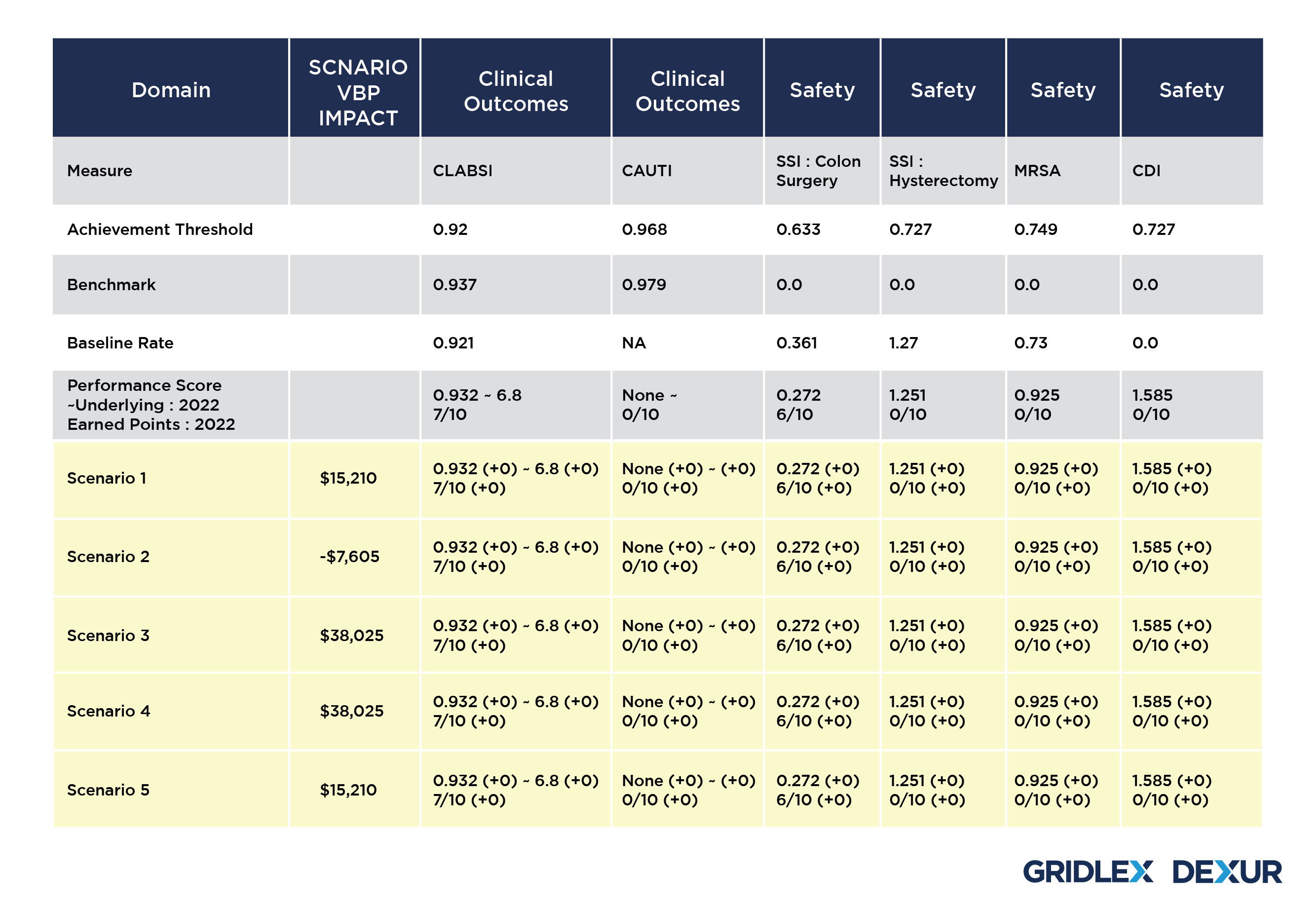
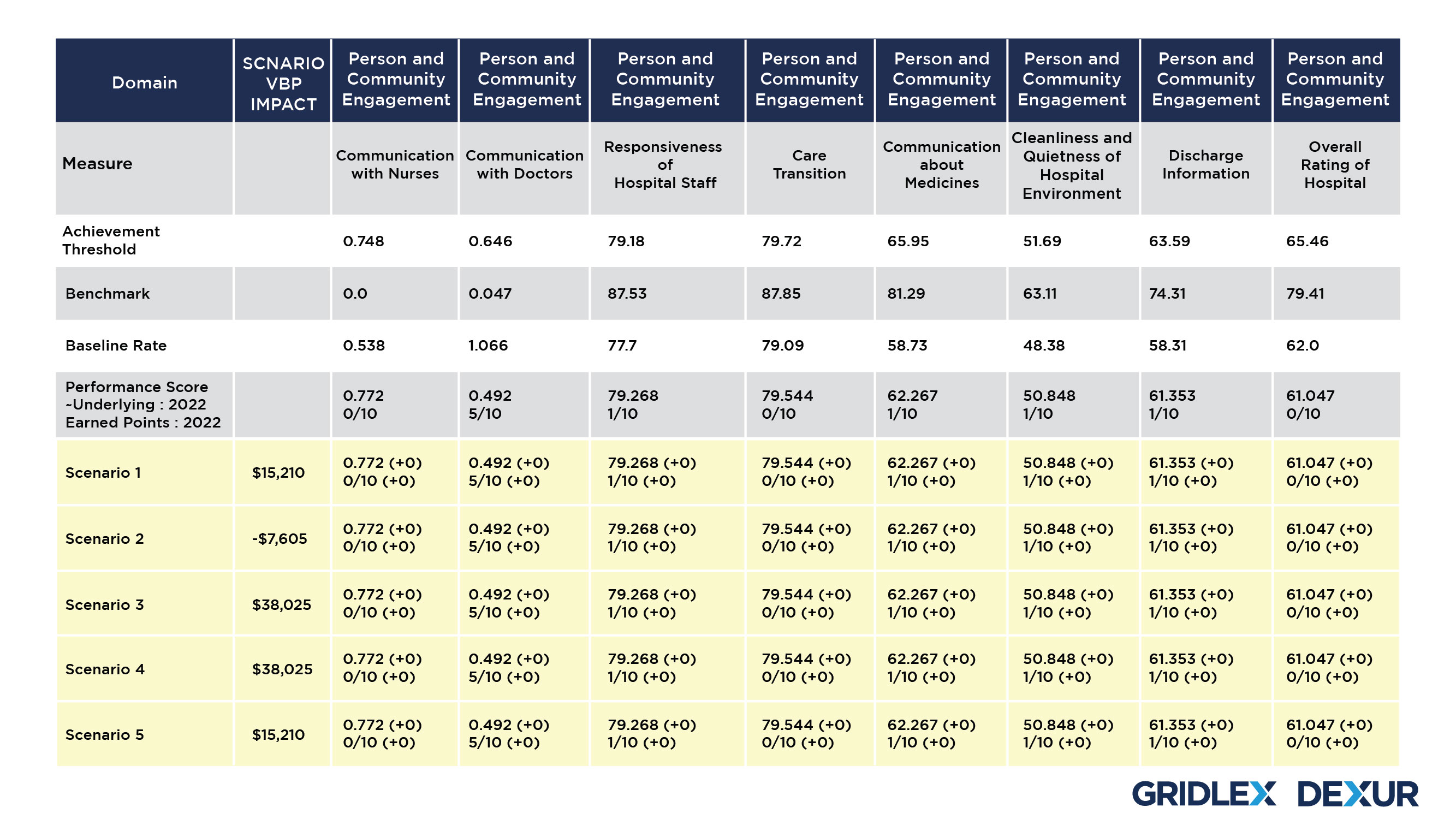
Dexur Simulator allows the Hospitals to choose a desired year and the amount of VBP impact. Based on the CMS Medicare claims data collected by Dexur, the simulator then runs 3 million simulations with all permutations for 18 VBP measures to come up with scenarios that suggest changes in different measures to be adopted by the Hospital.
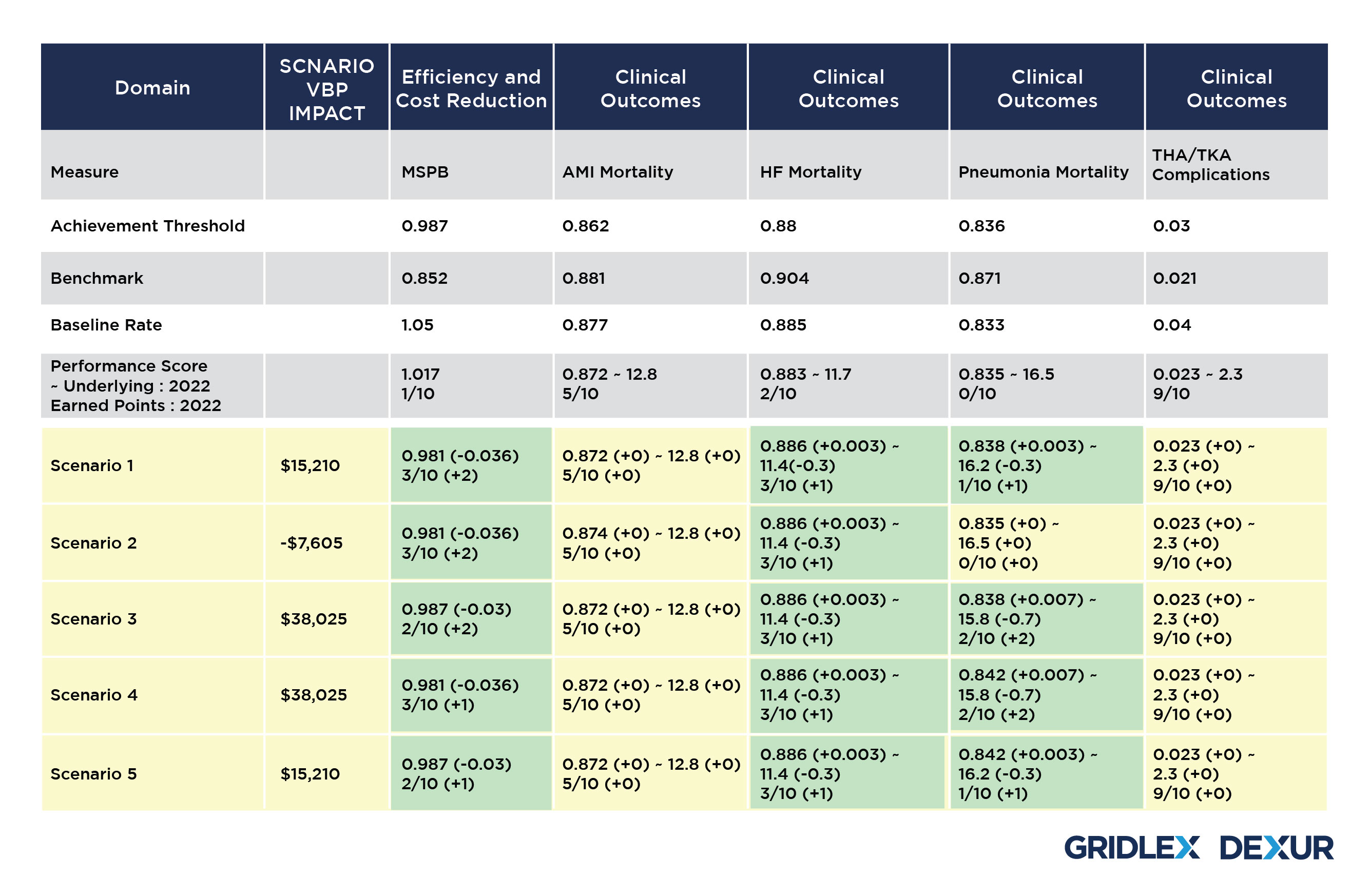
These scenarios are formulated using various combinations of changes in each VBP domain for improving the Performance Score for the Underlying year. Dexur’s Simulator uses Benchmarks and Achievement thresholds of the corresponding VBP Measure Time Periods to propose these changes. The adjustment in each of these domains subsequently creates a revision in the performance score, adding up to a total advancement in the Hospital’s VBP score to achieve the desired VBP Impact.
Additionally, Dexur simulator also provides the unique provision to use constraints on any of these domains. Based on the constraints applied in the domains and individual measures, a further customized result can be obtained.
VBP Manual Calculator
Dexur VBP manual calculator helps create various scenarios with changes in Hospital Performance for different VBP measures to get better incentives. Based on the selected fiscal year, the calculator provides various scenarios to adjust the Hospital Performance based on the corresponding Benchmarks and Achievement thresholds.
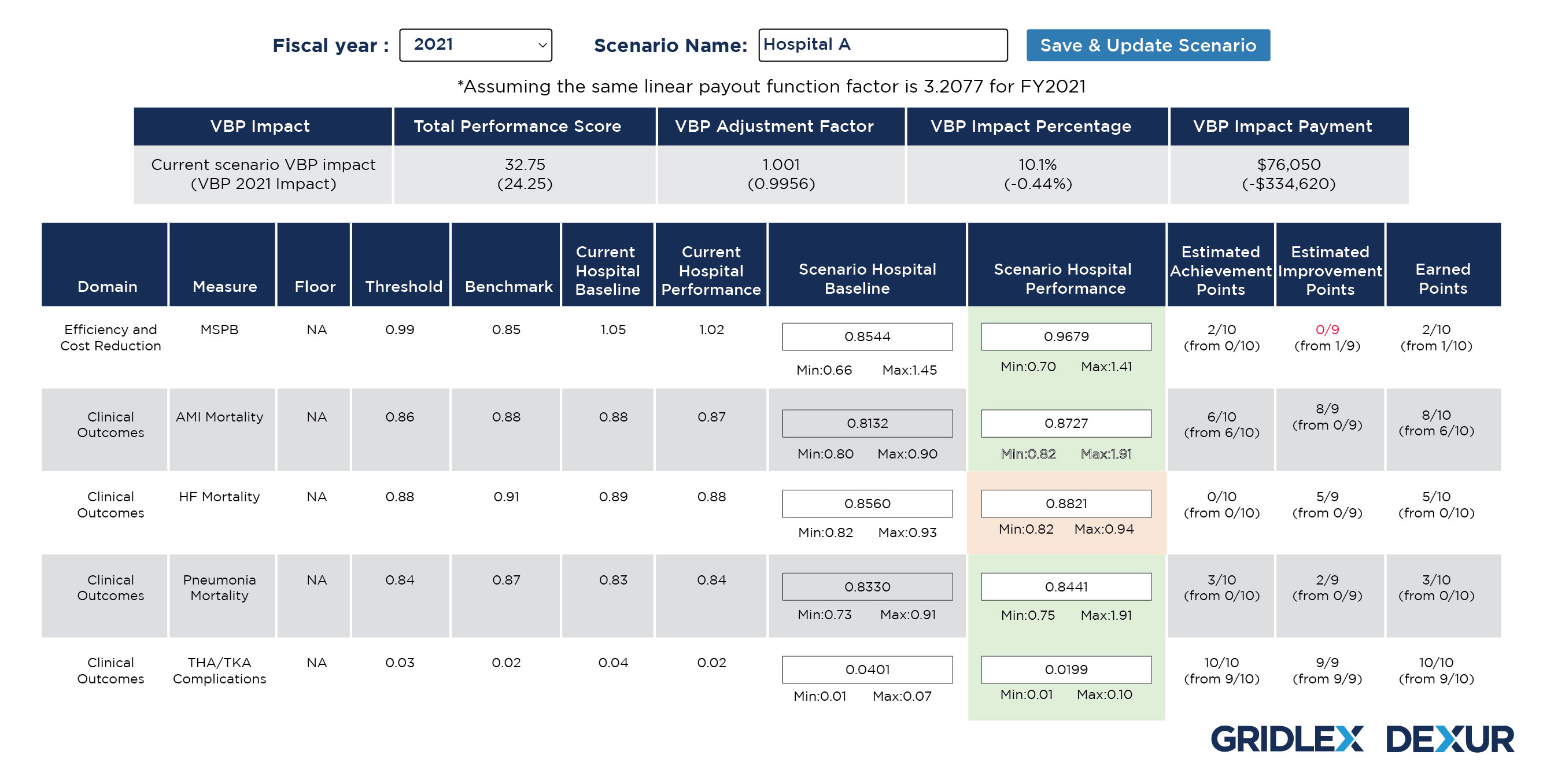
The Hospital Performance score values in each of the domain measures can be adjusted to improve the earned points in VBP. Adjusting the Hospital Performance score under various measures will help in calculating the VBP impact with any of the changes or its combinations.
Medicare Spending Per Beneficiary (MSPB)
MSPB is a significant factor in driving VBP payments as it accounts for 25% of overall VBP score. MSPB costs consist of costs incurring three days prior to hospitalization, index hospitalization costs, and 30 days post discharge cost. Minimizing the post index stay costs can reduce the average MSPB cost per episode to a large extent.
Dexur Calculator for MSPB Cost Reduction analyzes how reduction of post index stay costs can improve the VBP Adjustment Factor of hospitals. Post Index stay costs comprise of:
- Rehospitalizations
- Discharges to Skilled Nursing Facilities (SNF)
- Discharges to Home Health Agencies (HHA)
- Discharges to Home
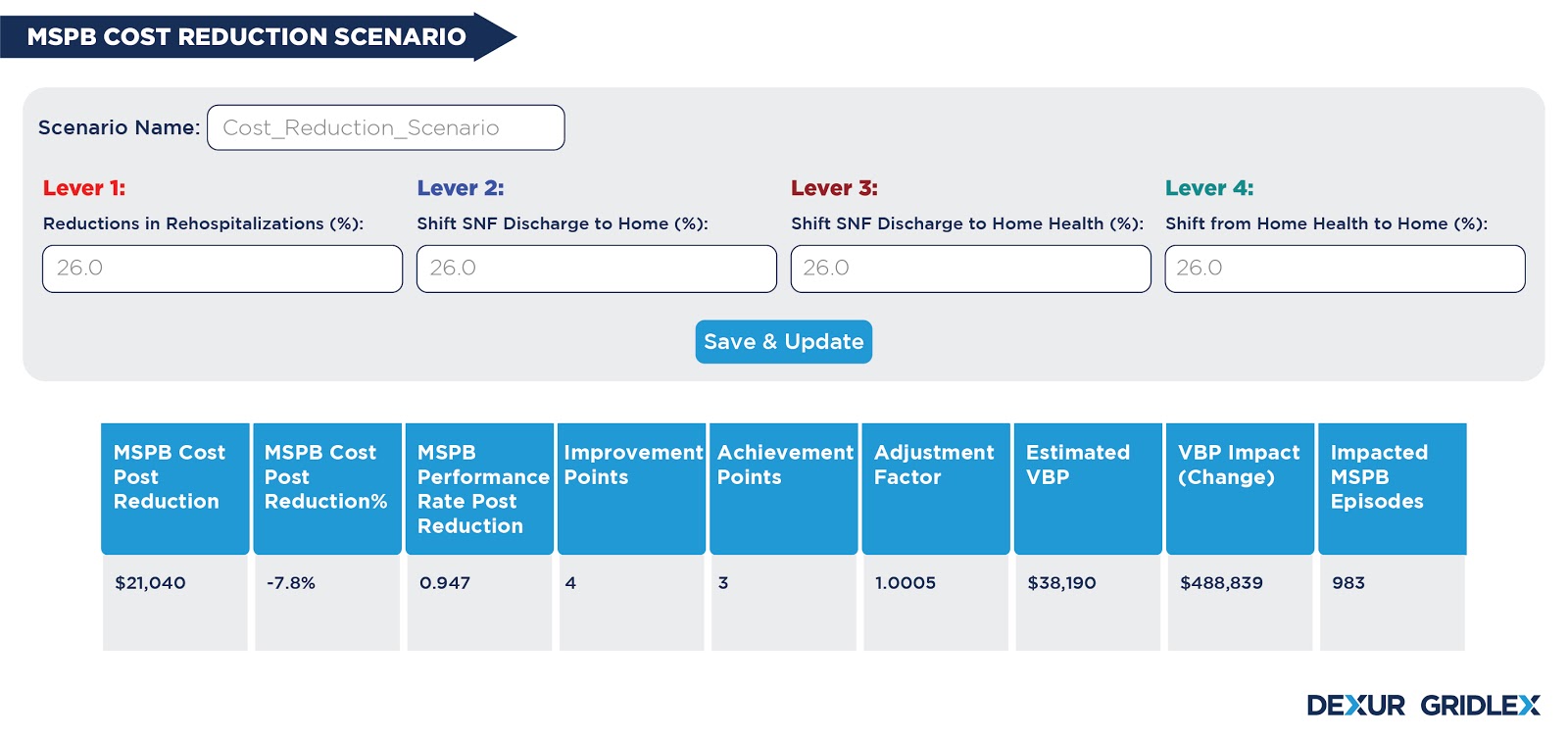
MSPB Cost Reduction Model
Dexur Calculator for MSPB Cost Reduction is designed to demonstrate the interaction between reduction in post index stay costs and its impact on average MSPB costs and VBP incentives. It assesses the post index stay costs, which are crucial in determining MSPB costs and has identified four main levers. The calculator estimates reduction in each of these levers to reduce overall MSPB cost.
- Lever 1: Reductions in Rehospitalizations
- Lever 2: Shift from SNF Discharge to Home
- Lever 3: Shift from SNF Discharge to Home Health
- Lever 4: Shift from Home Health to Home
The influence of post index stay costs reduction on VBP score is calculated by determining how reducing rehospitalizations or shifting a fraction of discharges, from one facility to another, could affect the overall MSPB cost. Value outcomes are listed in four levers, with percentage changes ranging from 5% to 100%.
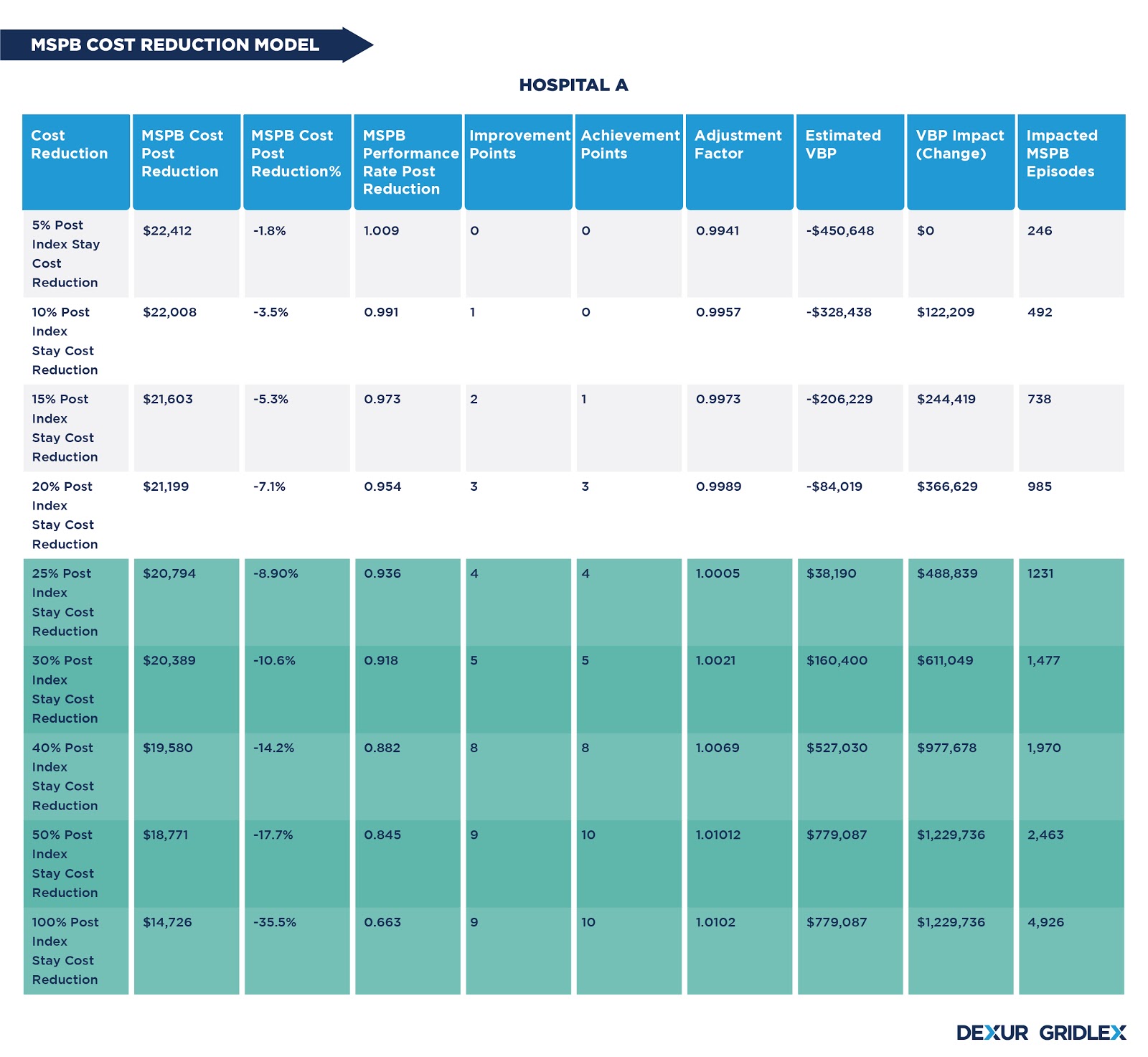
The cost to be reduced in each lever is determined by identifying the number of episodes affected by different percentage changes. Post index stay costs corresponding to the number of episodes is calculated and adjusted in each scenario. The cost reduction in different levers is dependent on the cost contribution of each post index stay facility to the MSPB costs. A higher reduction than the break-even point can further improve the VBP incentives.
MSPB Cost Reduction Scenario
Dexur Calculator for MSPB Cost Reduction also provides the unique facility to produce different scenarios for MSPB cost reduction manually. The tool helps to identify scenarios by which hospitals can adopt reduction in rehospitalizations or shifts in discharges by impacting the minimum number of episodes to avoid VBP penalties.
Dexur Calculator for HRRP Scenarios
The Hospital Readmissions Reduction Programme (HRRP) is a value-based purchasing program of CMS that aims at reducing avoidable hospital readmissions to enhance the national goal of improving healthcare. This is achieved by linking payments to the quality of hospital care. The payment reduction in HRRP is calculated by the CMS based on each hospital’s performance on a rolling three-year performance period. CMS reduces hospital payments based on payment adjustment factors. The payment reduction is capped at 3 percent (i.e., payment adjustment factor of 0.97).
Following are the six measures included in the program:
- Acute Myocardial Infarction (AMI)
- Coronary Artery Bypass Graft (CABG) surgery
- Chronic Obstructive Pulmonary Disease (COPD)
- Heart Failure (HF)
- Elective primary Total Hip Arthroplasty and/or Total Knee Arthroplasty (THA/TKA)
- Pneumonia
Each of these are procedure specific 30-day risk-standardized unplanned readmission measures.
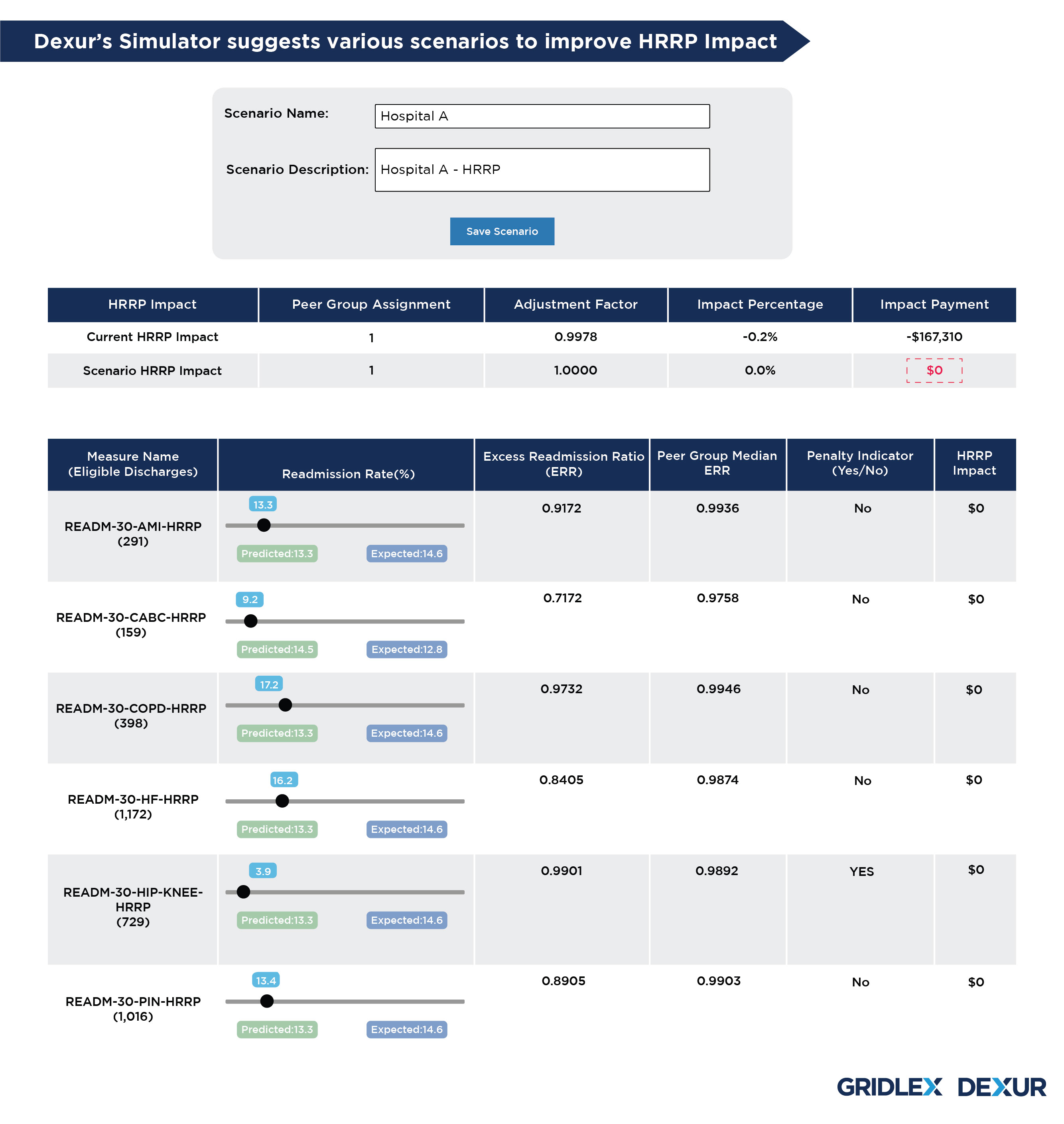
Dexur HRRP Scenarios
Being an approved purchaser of CMS Medicare claims data, Dexur replicates the CMS methodology to calculate HRRP impact payment of each hospital.
Step 1: Excess Readmission Ratio (ERR) is calculated for each measure.
Step 2: Hospitals are stratified into peer groups based on dual proportion. Median ERRs for each peer group are calculated.
Step 3: Each hospital's performance is compared to the peer group median ERR for each measure.
Step 4: Hospital's payment reduction is calculated.
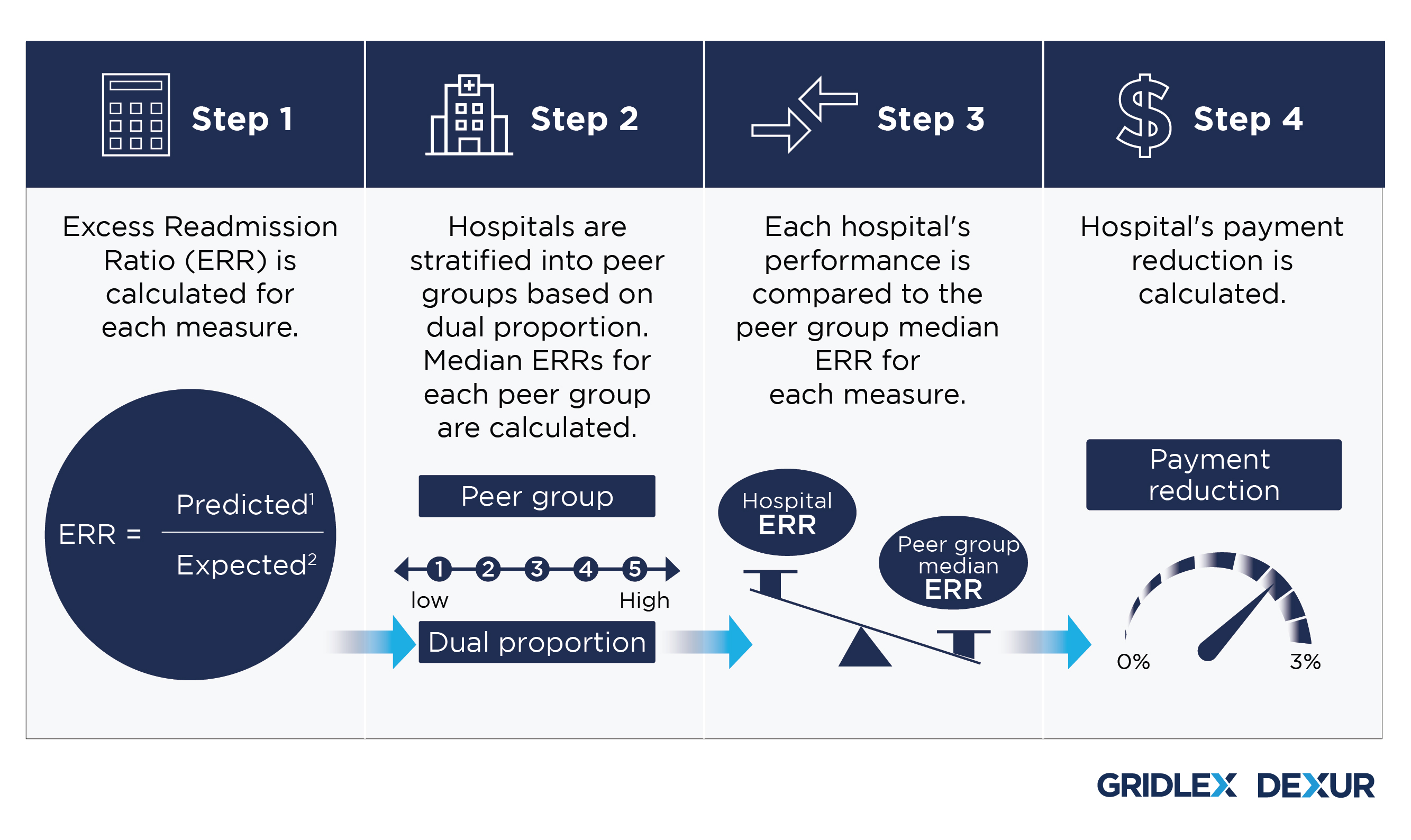
Apart from calculating HRRP payment impact, Dexur’s calculator helps create HRRP scenarios that reduce HRRP impact payment to $0 by improving the adjustment factor, which in turn helps avoid reduction in payments. The tool consists of sliders for all 6 measures, which can be manually adjusted to check the impact of desired readmission rate (%) of each measure on the payments. The tool also reflects the impact of change in readmission rate in the Excess Readmission Ratio (ERR) and HRRP adjustment factor.
This tool can be helpful for the hospitals in knowing their payment reduction from the HRRP program, creating scenarios for reducing the payment impact, and checking the impact of changes in readmission rate of individual measures on payment reduction and adjustment factor.
Dexur Calculator for HACRP Scenarios
Hospital Acquired Condition (HAC) refers to a medical condition acquired by a patient during the hospital stay, which was not present at the time of admission. The HAC Reduction Program (HACRP) is a value-based purchasing program of CMS that aims at improving healthcare quality by linking Medicare payments to hospitals’ performance on different measures in HAC. The HACRP adjusts payments to hospitals that rank in the worst-performing quartile (75th percentile) with respect to HAC quality measures, by making them subject to a 1 percent payment reduction.
CMS uses the Total HAC Score to determine the worst-performing quartile. For FY 2020, the Total HAC Score is based on data for six quality measures:
- CMS Recalibrated Patient Safety Indicator 90 (CMS PSI 90)
- Centers for Disease Control and Prevention (CDC) National Healthcare Safety Network (NHSN) Healthcare- Associated Infection (HAI) measures:
- Central Line-Associated Bloodstream Infection (CLABSI)
- Catheter-Associated Urinary Tract Infection (CAUTI)
- Surgical Site Infection (SSI) – colon and hysterectomy
- Methicillin-resistant Staphylococcus aureus (MRSA) bacteremia
- Clostridium difficile Infection (CDI)
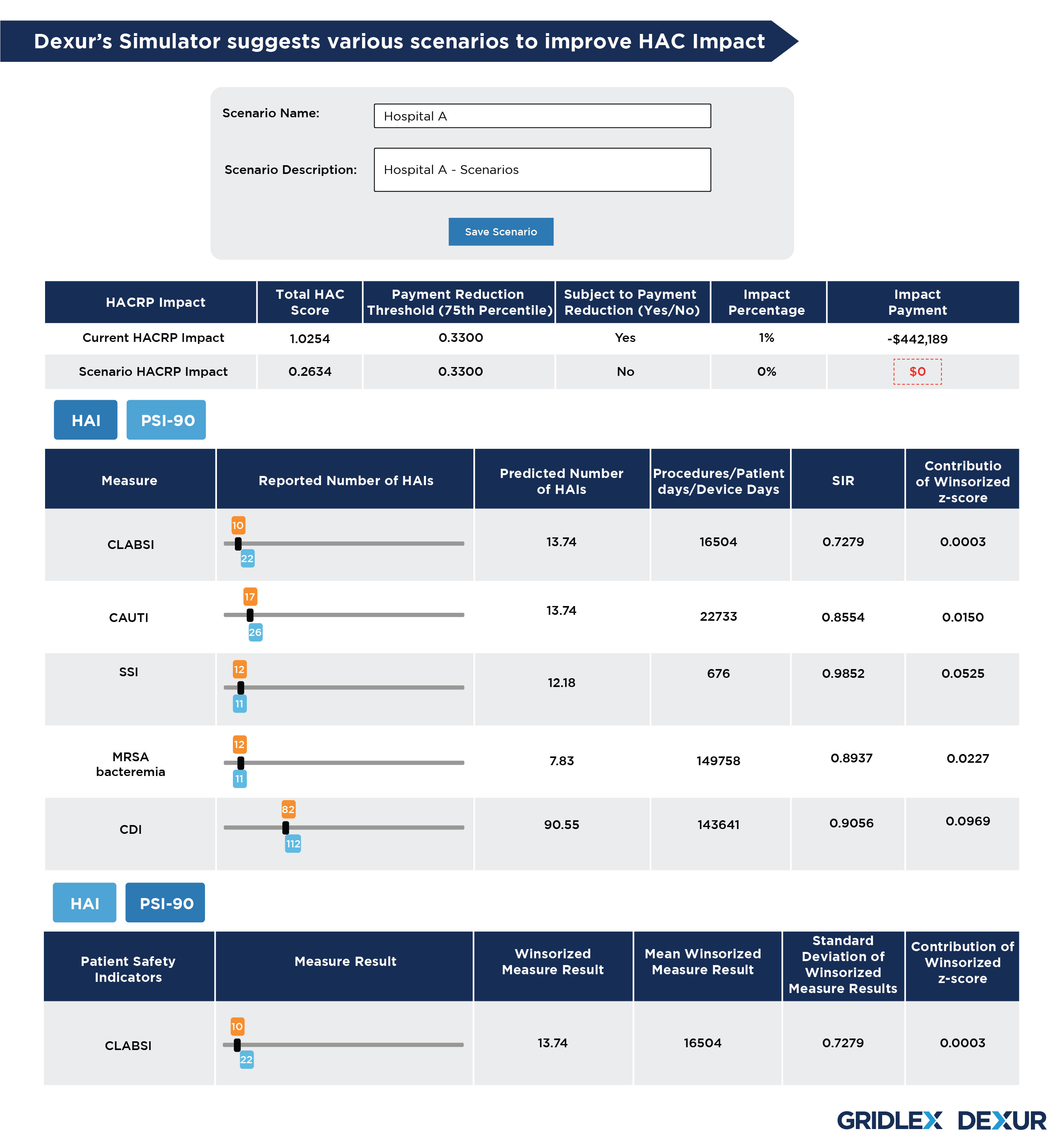
Dexur HAC Scenarios
Dexur’s calculator helps create HAC scenarios that reduce HACRP impact payment to $0 by improving the Total HAC Score, which in turn helps avoid reduction in payments.
Dexur estimates the magnitude of the HACRP penalty risk and identifies program measures that have the most influence on the Total HAC Score. The scenarios can be achieved by making adjustments in either or both of following two parts:
- HAI
- PSI - 90
HAI
The tool shows the reported number of HAIs, predicted number of HAIs, and Procedures/patient days/device days in the tool. The slider in the tool enables manual selection of any number of HAIs in order to check its impact on Standardized Infection Ratio (SIR). The resultant change in SIR and contribution of winsorized z-score is shown against each HAI measure.
PSI - 90
The tool also shows the measure result of CMS PSI - 90 composite and its contribution of winsorized z-score. The slider allows to check the impact of various measure results on the contribution of winsorized z-score, and its impact on the Total HAC score.
Determination of Impact Payment
CMS scoring methodology requires that equal weight should be applied to each measure for which a hospital has a measure score. Dexur calculates the winsorized z-scores (i.e., measure scores) for all measures including those where adjustments were made and Total HAC Score, by replicating CMS scoring methodology.
The scenario impact in the Total HAC Score shows whether the score is above or below the payment reduction threshold (75th percentile). A Scenario with Total HAC Score below the threshold can impact HACRP with no payment reduction.
Dexur Calculator for CMS Star Rating Scenarios
The Centers for Medicare & Medicaid Services (CMS) has devised a Five-Star quality rating system to gauge the experiences of Medicare beneficiaries with their healthcare providers. Based on various quality measures in five different categories, Hospitals are awarded a rating on a scale of 1 to 5, with 5 being the highest.
A combined score from all these measures gives an Overall Star Measure for the plan, where some measures are weighted more than others. CMS has developed this program to help the beneficiaries make a more informed decision related to healthcare by comparing hospitals based on quality ratings. A higher Star Rating indicates better quality and performance based on which the beneficiaries can choose hospitals and other healthcare providers in their area.
Dexur based on its replication of CMS Star Rating methodology, meticulously calculates each measure under different measure groups and provides data through multiple years. Dexur evaluates the performance of the hospitals based on its analysis of hospital values over previous and current years against their national average and median to make CMS Star predictions for the underlying year. Hospitals can use this data and focus on measures that need improvement to elevate their Star Rating and attract more medicare beneficiaries.
Dexur calculator for CMS Star Rating is a tool that helps in creating different scenarios by adjusting various quality measures under five different categories that impact CMS Star Rating:
- Mortality Measures (22 % Weightage)
- Readmission Measures (22 % Weightage)
- Safety of Care Measures (22 % Weightage)
- Patient Experience Measures (22 % Weightage)
- Timely and Effective Care Measures (12 % Weightage)
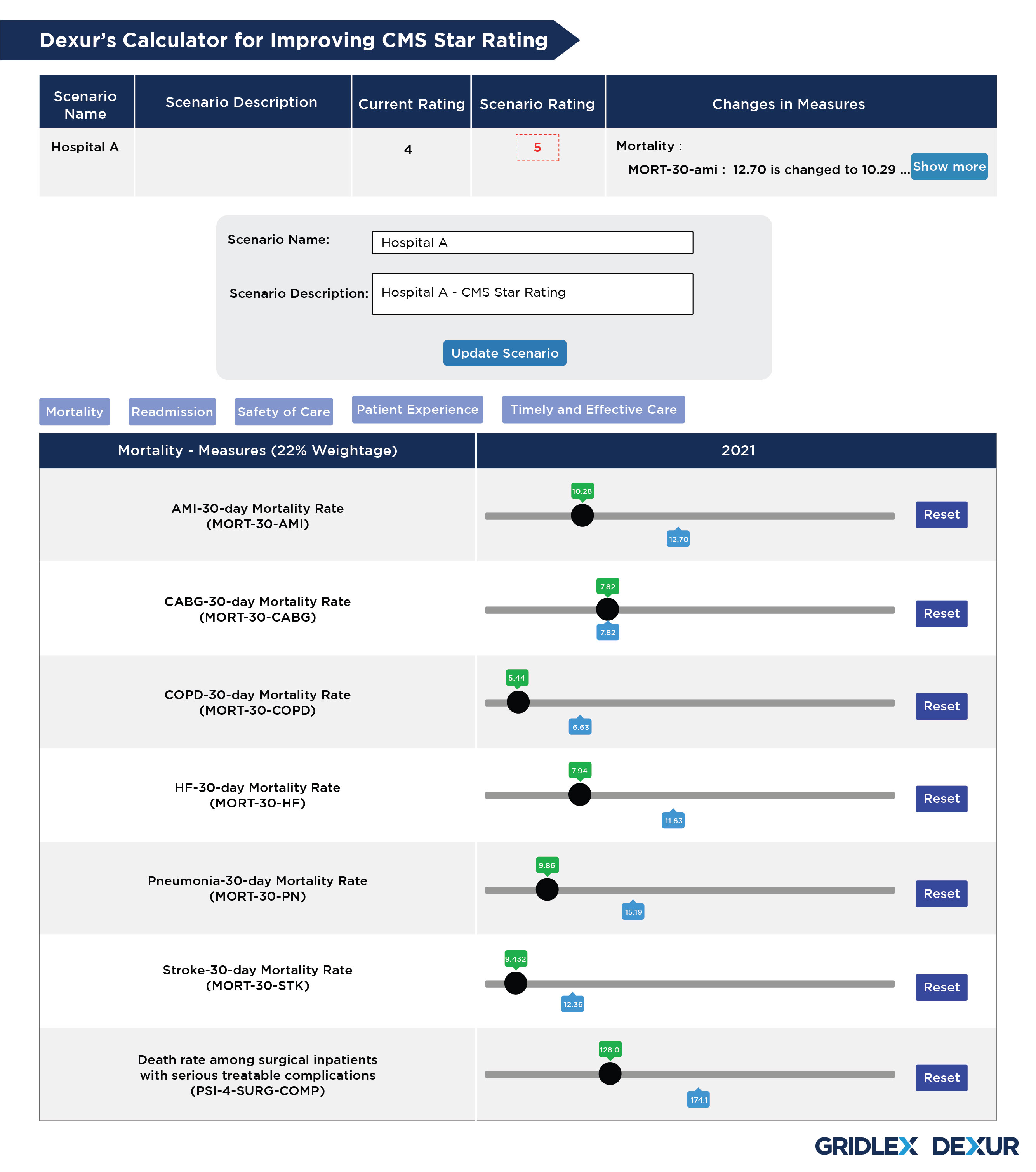
Dexur’s calculator consists of all 5 categories with values for different measures in the underlying year. These values are based on Dexur’s replication of complex CMS algorithms related to multiple measures involved. Dexur’s calculator allows the user to navigate through various measures in all categories and make desired changes. Based on the combinations of these changes made in each of these measures, the new values are added up to create a scenario and its corresponding CMS Star Rating. This will help the Hospital determine the measures to be taken to meet the standards prescribed by CMS to earn better quality ratings.
Similarly, using this tool, Hospitals can create multiple scenarios that tailor to their needs and demands. Based on the data obtained from these scenarios focusing on multiple measures, healthcare providers can improve their CMS Star Rating by narrowing down on individual factors and making necessary changes.