Get Dexur’s Personalized Hospital Specific Presentation on Quality, Safety, Compliance & Education
Latest Dexur News
All MBQIP Measures in One Place
The Medicare Beneficiary Quality Improvement Project (MBQIP) is a voluntary quality improvement initiative aimed at promoting better healthcare outcomes for patients treated in critical access hospitals (CAHs), which are often located in rural areas. MBQIP provides an opportunity for small hospitals to report on quality and outcomes data, fostering a culture of quality improvement and enhancing rural healthcare delivery.
Read moreUltrashort Readmissions are 30-40% of CMS 30 Day Readmission Measures
Ultrashort hospital readmissions, defined as patient readmissions within 7 days of discharge, present a significant challenge in healthcare management. These early readmissions not only reflect on the quality of care provided but also have substantial implications for patient safety and healthcare costs.
Read moreThe capacity for individualized patient care is a significant metric for healthcare quality and outcomes. In smaller rural hospitals, the scale of operations lends itself to a more personalized approach, particularly when managing chronic conditions such as heart failure (HF), acute myocardial infarction (AMI), pneumonia (PN), and chronic obstructive pulmonary disease (COPD). For these conditions, a typical rural hospital may see fewer than 200 patients over three years as per Centers for Medicare & Medicaid Services (CMS) measures, averaging about five patients monthly. This volume is distinctly manageable compared to larger systems, which often struggle to provide individualized follow-up care due to higher patient numbers.
Read moreCLABSI Case Study: Integrating Safety Huddles & Best Practices with Risk & Incident Management
Central Line-Associated Bloodstream Infections (CLABSIs) present a significant challenge in healthcare settings, critically impacting patient safety and care quality. These infections, often associated with the use of central lines in medical treatments, pose substantial risks, influencing key quality measures such as the NHSN (National Healthcare Safety Network) CLABSI metrics. This metric is integral to quality programs like the CMS Hospital CMS Star Rating, Hospital-Acquired Condition Reduction Program (HACRP). Leapfrog and other quality programs that influence hospital ratings and funding. CLABSIs are not only a patient safety risk concern but also a quality indicator, affecting a hospital's performance evaluation and reputation.
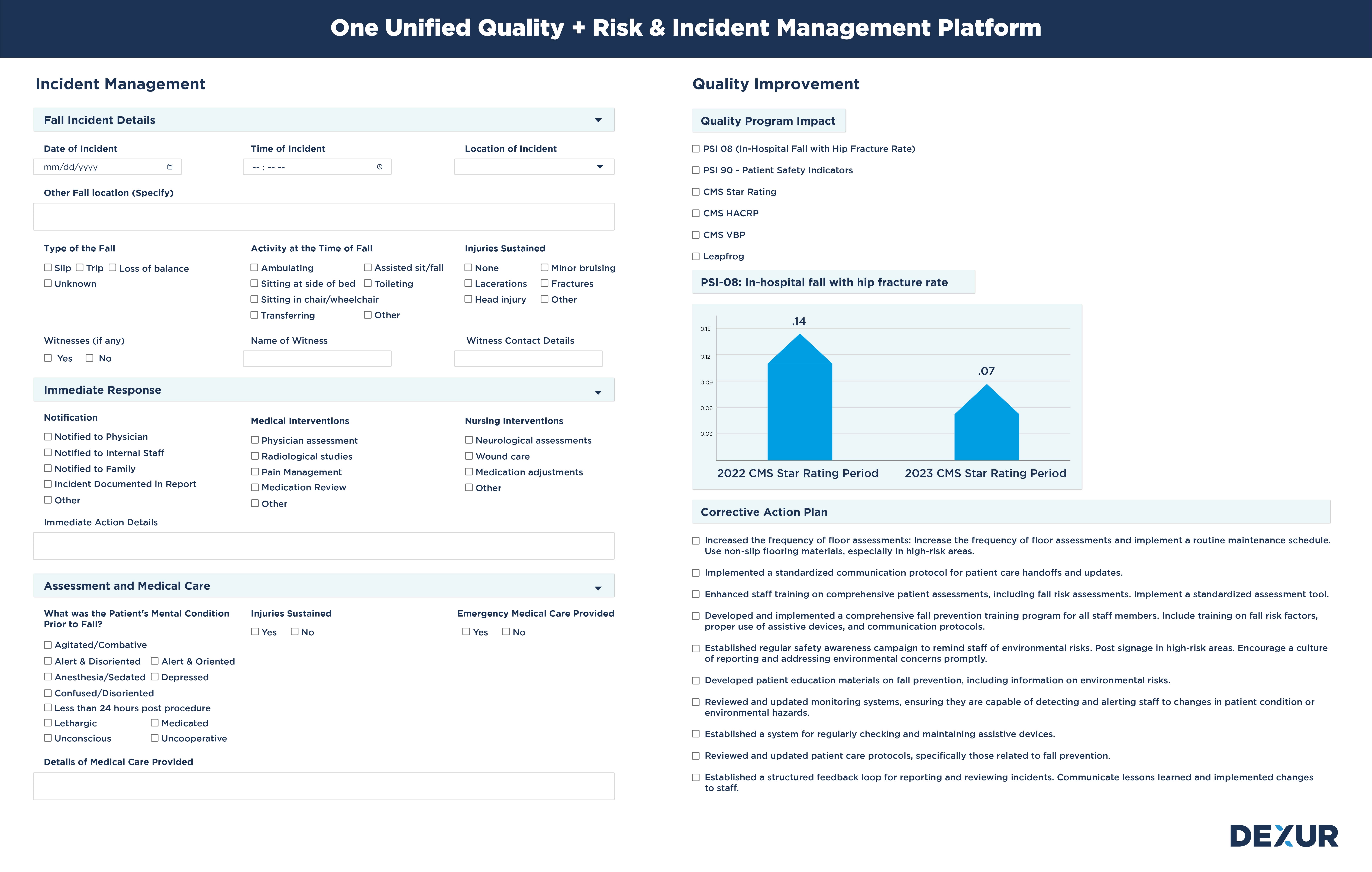
Read morePatient Falls: Case Study: Quality and Risk are Two Sides of the Same Coin
Patient falls within healthcare settings are a significant concern due to their implications on patient safety and quality of care. These incidents have an impact on risk management and also have an impact on measures like PSI 08 (In-Hospital Fall with Hip Fracture Rate) which is part of PSI 90, which influence crucial quality programs including CMS Star Ratings, the Hospital-Acquired Condition Reduction Program (HACRP), and Leapfrog standards. PSI 90, or the Patient Safety and Adverse Events Composite, encompasses a range of hospital-acquired conditions, among which patient falls are a critical component. The impact of falls on these quality measures is profound, as they directly affect a hospital's reputation, funding, and overall performance evaluation.
Read moreThe Big Picture in Infection Prevention: Beyond Day-to-Day Operations
Infection Prevention teams in hospitals play a critical role in maintaining patient safety and healthcare quality. Their work, often seen through the lens of daily tasks and immediate outcomes, holds a far greater significance in the broader context of healthcare delivery and institutional reputation. To fully grasp the impact of their efforts, it's essential for these teams to understand the big picture, much like the famous story of a civil engineer who, when asked about their job, said they were not just building walls and roofs but a beautiful building. This narrative underscores the importance of seeing beyond the immediate task to appreciate the larger purpose and impact of one’s work.
Read moreHospitals Need To Introduce and Adopt The Concept of Readmission and Mortality Huddles
Hospitals seeking to enhance healthcare quality and patient safety have adopted strategies like the 'Safety Huddle,' a collaborative session focusing on patient safety concerns. Evolving from this concept is the 'Readmission and Mortality Huddle,' an interdisciplinary team meeting specifically aimed at analyzing readmissions and mortalities. This focused approach is crucial in the light of Dexur's findings about the narrow scope for improvements in healthcare metrics. The goal of these huddles is to identify patterns, discern root causes, and devise prevention strategies, with frequent and concise meetings enabling prompt interventions and ongoing monitoring, marking a significant advancement in hospital management.
Read moreDexur's AI Advisor Shows Quality Improvement is a Game of Inches
Dexur had already previously published that the difference between the Bottom 10th & top 90th Performance Percentiles of CMS Readmission and Mortality Measures is Very Small. Dexur’s AI Advisor can automatically analyze a Hospital’s data and give very specific goals and counts on what it takes for Hospitals to get to the top 90th percentile. Dexur’s AI Advisor's findings suggest that for many hospitals, reducing readmissions and mortalities by less than 10 per year can significantly boost their percentile ranking. This revelation is crucial as it indicates that even minor improvements can lead to substantial gains in a hospital's performance metrics.
Read moreHospital Incident Management Systems: A Wasted Opportunity to Integrate Quality Metrics
Hospital Incident Management Systems are widely adopted across healthcare organizations to capture, track, and manage events that could potentially harm patients, employees, or the institution. Although these systems play a crucial role in identifying and mitigating risk, they often function in isolation from Quality Management Systems. As a result, there's a missed opportunity to integrate quality goals and measures such as the CMS Star Rating, Leapfrog Hospital Safety Grade, Hospital Readmissions Reduction Program (HRRP), Hospital-Acquired Condition Reduction Program (HACRP), and Value-Based Purchasing (VBP).
Read moreSmall Size as an Advantage for Rural Hospitals: Smart Use of Technology + Manual Approaches
In the healthcare industry, large organizations face significant challenges due to their size and complexity. Cross-departmental coordination is a critical requirement to mitigate risk, often leading to bureaucratic inertia. Large hospitals rely on massive, centralized systems designed for economies of scale, but these can be slow and costly to alter. When faced with problems, these institutions typically turn to technology as a solution, inflating capital expenditure (Capex) budgets and return on investment (ROI) benchmarks, thus creating barriers to change.
Read moreRural hospitals, with their smaller size, often face the challenge of limited budgets and resources compared to larger healthcare institutions. Large organizations typically have the luxury to allocate distinct technology and application budgets across various functional departments like Quality, Compliance, Risk, and Learning. Each department independently evaluates and selects applications tailored to its unique needs, an approach that often leads to additional spending on system integration to ensure cross-departmental compatibility.
Read moreAll MBQIP Measures in One Place
The Medicare Beneficiary Quality Improvement Project (MBQIP) is a voluntary quality improvement initiative aimed at promoting better healthcare outcomes for patients treated in critical access hospitals (CAHs), which are often located in rural areas. MBQIP provides an opportunity for small hospitals to report on quality and outcomes data, fostering a culture of quality improvement and enhancing rural healthcare delivery.
Read moreRural Health and The Challenges of Low Case Volume: MRSA Case Study
Rural hospitals are essential cornerstones of the communities they serve, yet they face unique challenges in assessing the quality of healthcare services they offer. One significant challenge arises from low patient volumes which, while potentially indicative of effective healthcare or healthier populations, can distort quality metrics. This distortion makes benchmarking performance against national standards a complex endeavor. Through the lens of MRSA (Methicillin-resistant Staphylococcus aureus) infections, we can gain valuable insight into this issue.
Read moreEnhance Employee Learning and Training for Improved Performance and Compliance with Dexur
Holistic Approach to Automated Assessments & Grading
Dexur’s platform takes a holistic approach to Employee Learning and Training, covering a wide range of topics from professional skills development to regulatory compliance. Our automated assessments and grading systems ensure that employees meet the standards set across different domains, from quality care measures to compliance with legal regulations like OSHA standards.
Read moreElevate Quality Outcomes through Targeted Education with Dexur
Automated Assessments & Grading in Quality Outcomes Education
Quality Outcomes Education is integral to improving performance in healthcare metrics. Dexur's platform automates assessments and grading within Quality Outcomes Education programs. This streamlines the process, linking it directly to important metrics like CMS Star Ratings, Leapfrog Scores, Value-Based Purchasing (VBP), Readmissions, and Mortality rates.
Read moreStreamline Continuing Education for Improved Quality Metrics with Dexur
Automating Continuing Education Assessments & Grading
Continuing Education (CE) is critical not only for the professional growth of healthcare staff but also for quality outcomes. Dexur's platform automates the assessments and grading of Continuing Education programs, eliminating the manual bottlenecks. Automated assessments are synced with performance metrics like CMS Star Ratings, Leapfrog Scores, and Value-Based Purchasing (VBP) programs, enabling a seamless data-driven approach to education.
Read moreReal-Time Reporting Capabilities
Traditional compliance reporting processes often suffer from delays and manual bottlenecks. Dexur’s platform revolutionizes this by offering real-time reporting features. Our system integrates seamlessly with your existing infrastructure, pulling data from various sources to populate compliance reports automatically. This ensures you always have the most current and comprehensive information at your fingertips.
Read moreElevate Compliance Risk Assessment with Dexur's All-in-One Solution
Comprehensive Risk Analysis
Identifying compliance risks is the first step in mitigating them. Dexur's unified platform provides an all-encompassing risk assessment module, enabling you to pinpoint vulnerabilities across the organization. Our advanced analytics assess risk factors, both obvious and subtle, offering a complete view of your compliance landscape.
Read moreStreamline Policy Management with Dexur's Unified Platform
Optimize Policy Creation and Implementation
Creating and maintaining policies is a critical task that has a direct impact on an organization's quality and compliance. Dexur’s platform integrates seamlessly with your existing systems to create a unified solution. Utilize our platform to simplify the process of drafting, reviewing, and approving policies. Our intuitive workflow ensures that all team members are aligned, and policies are consistent across the board.
Read moreStreamlining Infrastructure Incident Management with Dexur
The Scope of Infrastructure Incidents
Incidents related to healthcare facility infrastructure, such as equipment malfunction, drug diversion, and utility failures, can have a cascading effect on patient safety and operational efficacy. Dexur’s unified platform serves as an integrated solution for monitoring, documenting, and resolving these incidents. Its robust analytics also allow for trend identification, providing a more strategic approach to incident management.
Read more