Sepsis Involved in 22% of In-Hospital Deaths in Hepatocellular Carcinoma Patients
In Hepatocellular Carcinoma (HCC)
Get Dexur’s Personalized Hospital Specific Presentation on Quality, Safety, Compliance & Education
By: James Pitt Nov. 28, 2018
Sepsis is a major killer of hepatocellular carcinoma patients. In the last five years, 22% of in-hospital deaths among Medicare inpatients with HCC involved severe sepsis.
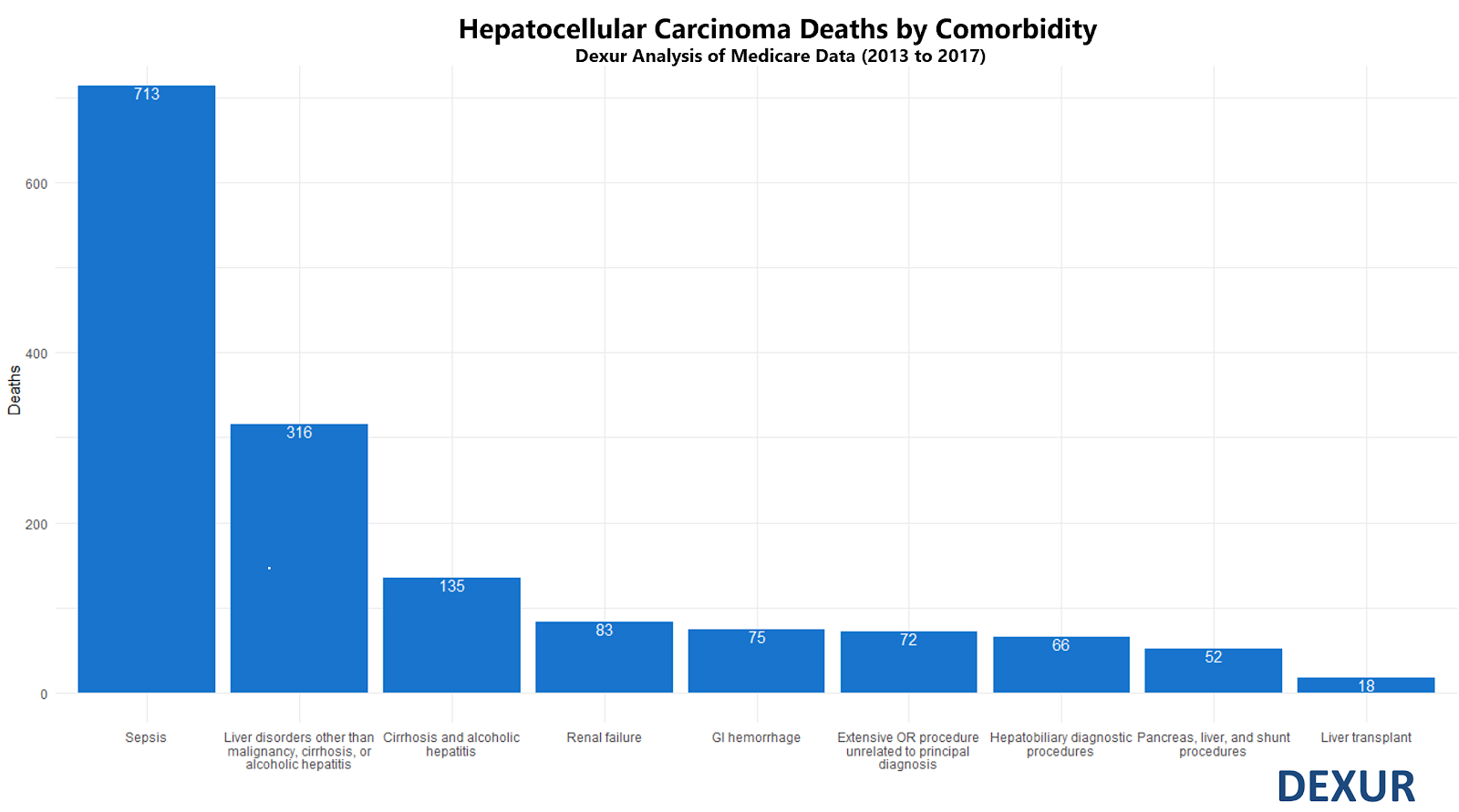
There were 3,180 in-hospital deaths in Medicare inpatients with HCC as a primary or secondary diagnosis code from 2013 to 2017, of which 713 involved severe sepsis. No other diagnosis codes were associated with such a high proportion of deaths in HCC patients.
The percentage of HCC deaths that involve severe sepsis appears to exceed the percentage of overall cancer deaths that involve severe sepsis. According to Williams et. al (2004), 8.5% of cancer deaths overall involve severe sepsis.
Why is sepsis such a danger to HCC patients? Pre-existing liver dysfunction creates vulnerability to sepsis, and liver injury is associated with worse sepsis outcomes. According to Yan et. al (2014), “Mortality rates among sepsis patients with liver dysfunction or failure range from 54% to 68%, higher than the mortality rates of sepsis patients with respiratory system dysfunction or failure.”
Bacterial infections are common and lethal in patients with liver disease. Bajaj et. al (2012) report that “Up to one-third of all hospitalised patients with cirrhosis are infected. With sepsis, mortality increases to more than 50%”
Yan et. al attribute this in part to liver-mediated immunosuppression. “T cells are exposed to an immunosuppressive microenvironment in the liver, which includes suppressive cytokines such as IL-10, transforming growth factor-β, and inhibitory molecules such as PD-L1 produced by [antigen-presenting cells].”
The intersection of sepsis and oncology is well-studied, because cancer patients are often immunosuppressed. Early diagnosis can be difficult; infections in cancer patients may present with more fever but fewer other inflammatory symptoms than in other patients. A 2016 presentation from the Sidney Kimmel Cancer Center at Johns Hopkins provides updated screening recommendations.
To reduce the likelihood of infection, the October 2018 ASCO guideline update provides antimicrobial prophylaxis recommendations for cancer patients, which can help prevent sepsis. (As a side note, these recommendations include treatment with a nucleoside reverse transcription inhibitor in patients at risk of hepatitis B virus reactivation. This risk is very pertinent for HCC patients, as HBV is associated with 80% of HCC cases worldwide, and 20% in Western countries).
Once sepsis has been detected, the 2014 AGIHO guidelines on management of sepsis in neutropenic patients stress urgent treatment. “Empirical antimicrobial treatment using broad-spectrum antibiotics must be started immediately… each hour of delay in antimicrobial administration over the ensuing 6 h was associated with an average decrease in survival of 7.6 %.” Liver damage impairs drug clearance; Park et. al (2015) recommend intravenous third generation cephalosporins, and Bartoletti et. al (2018) recommend beta-lactams as first-line therapy. Both stress the need to be aware of multi-drug resistant pathogens.
Future directions in sepsis treatment may include immunoadjuvant therapy. In August 2018, Watanabe et. al reviewed checkpoint inhibition as a sepsis control strategy. Two PD-1 pathway inhibitors have passed Phase I safety trials for sepsis, BMS-936559 and nivolumab. PD-1 inhibition has also been approved for use against HCC itself. However, PD-1 inhibitors are not currently undergoing later-phase trials for sepsis treatment.
ABOUT THE AUTHOR
