How to Evaluate the Impact of Fluid Imbalances on Sepsis Patients: Part 2: Length of Stay
In Fluid Imbalance
Get Dexur’s Personalized Hospital Specific Presentation on Quality, Safety, Compliance & Education
By: James Pitt Jul. 25, 2018
Mortality rates are the most important outcome in sepsis patients. However, outcomes short of mortality matter both for patient well-being and for hospital costs.
Fluid overload is associated with longer length of stay (LOS). A 2015 study of critically ill patients in general found that those with fluid overload had an average LOS of 11.5 days, as opposed to 8 days for patients without fluid imbalance. Dexur has previously found an association between fluid imbalance and LOS in sepsis patients. Fernando et. al 2018 found care for sepsis patients had a mean cost per day of $3,536 (in direct admits) to $3,813 (in transfers). Reducing length of stay can help reduce hospital costs.
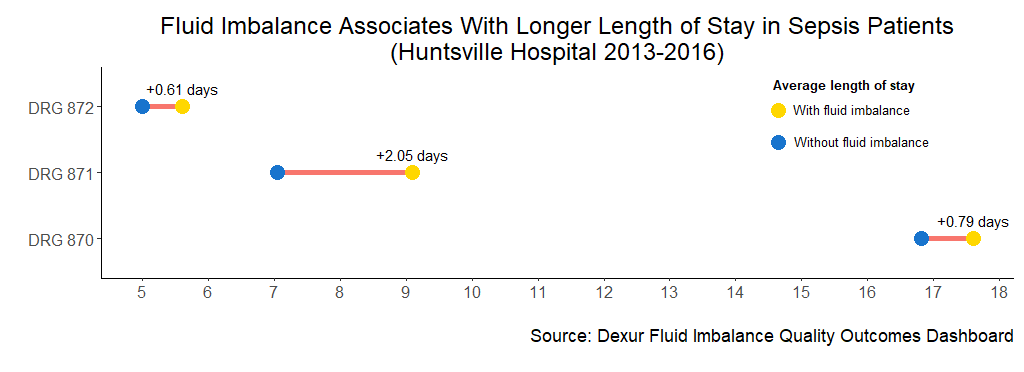
Dexur analysts examined length of stay in sepsis patients with and without fluid imbalance at Huntsville Hospital (AL), as a case study in how hospitals can evaluate the potential value of fluid imbalance interventions at their institution. At Huntsville Hospital, fluid imbalance was associated with longer average length of stay in all sepsis patients. The increase was largest in sepsis patients with major complications with less than 96 hours of mechanical ventilation (DRG 871). In this subgroup, patients with fluid imbalance averaged 2.05 days longer in-hospital than patients without fluid imbalance.
The most recent update of the Surviving Sepsis Bundle, in June 2018, cautions that “fluid administration beyond initial resuscitation requires careful assessment of the likelihood that the patient remains fluid responsive.” This update responds to several studies that report a link between positive fluid balance and mortality. Earlier versions of the Surviving Sepsis Bundle called for “early goal-directed therapy,” including aggressive fluid administration that could lead to fluid overload. Meta-analysis did not support this approach.
ABOUT THE AUTHOR
