Over Half of DRG 871 Urosepsis Discharges had Fluid Imbalances in Top 5 Connecticut Hospitals
In Fluid Imbalance
Get Dexur’s Personalized Hospital Specific Presentation on Quality, Safety, Compliance & Education
By: James Pitt May. 22, 2018
Sepsis is a common and severe complication of infection. It is frequently comorbid with urinary tract infections (UTIs), a condition called urosepsis. A 2015 study of 5,272 sepsis cases in intensive care found that nearly 20% of cases stemmed from a urinary infection.
Fluid balance is an important part of sepsis treatment. Early fluid administration is important to prevent hypovolemia, but fluid overload is dangerous. Sakr et. al (2005) found that sepsis patients with higher cumulative fluid imbalance had more acute lung injury or acute respiratory distress syndrome - and an elevated risk of mortality even after controlling for those pulmonary effects. Since UTIs interfere with urination, they, of course, make removing fluid from the body more difficult. Devices that monitor hemodynamic variables such as cardiac output and stroke volume variation can help guide fluid administration.
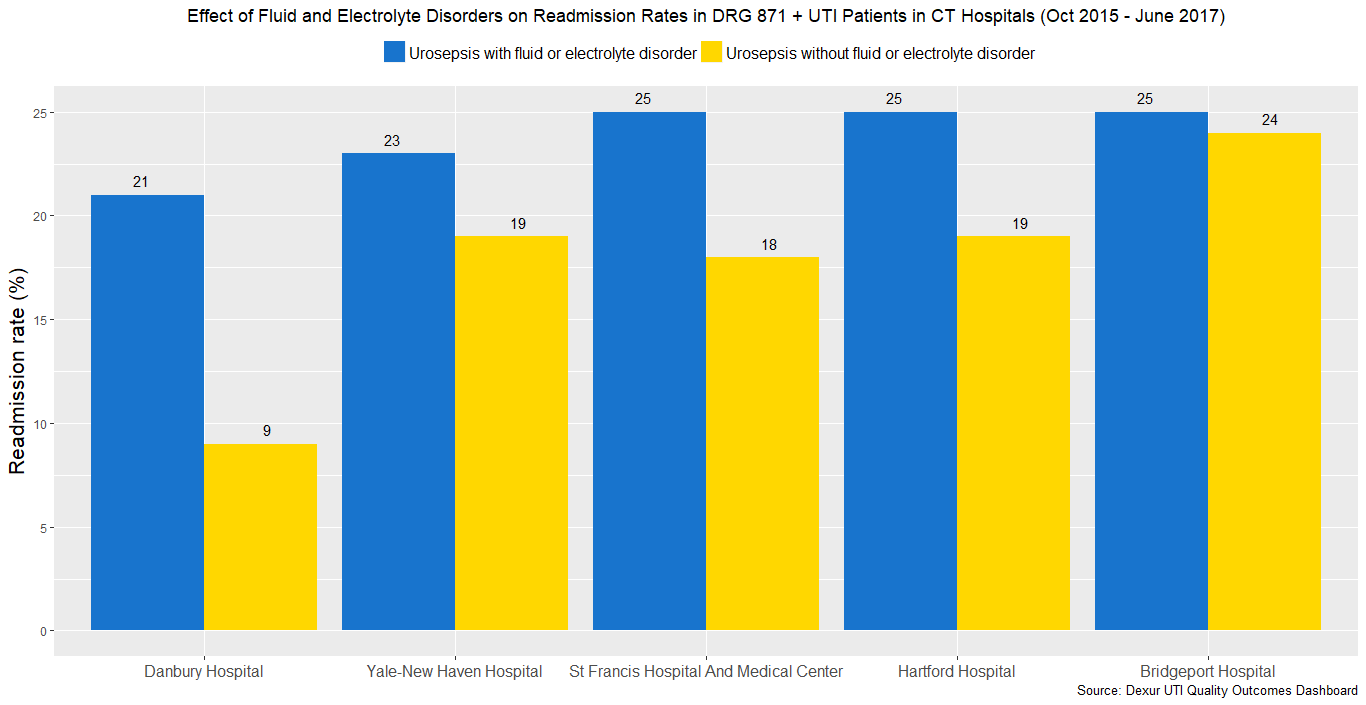
Dexur analysts examined CMS discharge data to study the impact of fluid imbalance in urosepsis patients. The sample consisted of patients with UTIs and sepsis at the five largest hospitals in Connecticut from October 2015 to June 2017. In all five of these hospitals, more than half of patients who had UTIs and sepsis with major complications or comorbidities (DRG 871) also had a fluid or electrolyte disorder, indicating they had a fluid imbalance.


After excluding patients who expired, were transferred, or were discharged against medical advice, over 50% of DRG 871 urosepsis patients at these hospitals also had a fluid or electrolyte disorder. The rate of fluid or electrolyte disorders in these patients was 77% at St. Francis Hospital and Medical Center (Hartford), 68% at Danbury Hospital, 63% at Yale-New Haven Hospital, 62% at Hartford Hospital, and 58% at Bridgeport Hospital.
Patients with fluid and electrolyte disorders were more likely to be readmitted than other urosepsis patients. Better fluid balance monitoring could reduce the percentage of sepsis patients who end up with fluid and electrolyte disorders. This could, in turn, reduce readmission rates.
- Total Discharges with DRG 871, UTI & Fluid and electrolyte disorders
- Total Discharges after Exclusion with DRG 871, UTI & Fluid and electrolyte disorders
- Total Readmissions with DRG 871, UTI & Fluid and electrolyte disorders
- Readmission Rate with Fluid and electrolyte disorders
- Total Discharges with DRG 871 & UTI
- Total Discharges after Exclusion with DRG 871 & UTI
- Total Readmissions with DRG 871 & UTI
- Readmission Rate with DRG 871 & UTI
- Inferred readmission rate without fluid imbalance
- Percent of discharges with DRG 871 and UTI who also have fluid and electrolyte disorder
From October 2015 to June 2017, for Yale-New Haven Hospital (New Haven, CT), Hartford Hospital (Hartford, CT), St. Francis Hospital and Medical Center (Hartford, CT), Danbury Hospital (Danbury, CT), and Bridgeport Hospital (Bridgeport, CT).
ABOUT THE AUTHOR
